Flaws in C Pandemic Theory
Prepare For Change / Derek Knauss

In depth research as provided by one of our subscribers:
David Crowe
Version 8.5. June 6, 2020
https://theinfectiousmyth.com/book/CoronavirusPanic.pdf
1. Executive Summary
The world is suffering from a massive delusion based on the belief that a test for RNA2 is a test for a deadly new virus, a virus that has emerged from wild bats or other animals in China, supported by the western assumption that Chinese people will eat anything that moves.
If the virus exists, then it should be possible to purify viral particles. From these particles RNA can be extracted and should match the RNA used in this test. Until this is done it is possible that the RNA comes from another source, which could be the cells of the patient, bacteria, fungi etc. There might be an association with elevated levels of this RNA and illness, but that is not proof that the RNA is from a virus. Without purification and characterization of virus particles, it cannot be accepted that an RNA test is proof that a virus is present.
Definitions of important diseases are surprisingly loose, perhaps embarrassingly so. A couple of symptoms, maybe contact with a previous patient, and a test of unknown accuracy, is all you often need. While the definition of SARS, an earlier coronavirus panic, was self-limiting, the definition of COVID-19 disease is open- ended, allowing the imaginary epidemic to grow. Putting aside the existence of the virus, if the COVID-19 test has a problem with false positives (as all biological tests do) then testing an uninfected population will produce only false-positive tests, and the definition of the disease will allow the epidemic to go on forever.
This strange new disease, officially named COVID-19, has none of its own symptoms. Fever and cough, previously blamed on uncountable viruses and bacteria, as well as environmental contaminants, are most common, as well as abnormal lung images, despite those being found in healthy people. Yet, despite the fact that only a minority of people tested will test positive (often less than 5%), it is assumed that this disease is easily recognized. If that were truly the case, the majority of people selected for testing by doctors should be positive.
The COVID-19 test is based on PCR, a DNA manufacturing technique. When used as a test it does not produce a positive/negative result, but simply the number of cycles
1 Officially the virus is called SARS-CoV-2 and the disease it is believed to caused, COVID-19. We will just refer to COVID-19 for the current virus panic, and SARS for the 2003 panic.
2 Ribonucleic Acid (RNA) is chemically very similar to DNA, except that one of the four bases, Thymine, is replaced by Uracil. In function it is very different, being created from DNA for a temporary use such as creating a protein molecule. It is also found in a single strand rather than a double-helix.
required to detect sufficient material to beat the arbitrary cutoff between positive and negative. If positive means infected and negative means uninfected, then there are cases of people going from infected to uninfected and back to infected again in a couple of days.
A lot of people say it is better to be safe than sorry. Better that some people are quarantined who are uninfected than risk a pandemic. But once people test positive, they are likely to be treated, with treatments similar to SARS. Doctors faced with what they believe is a deadly virus treat for the future, for anticipated symptoms, not for what they see today. This leads to the use of invasive oxygenation, high dose corticosteroids, antiviral drugs and more. In this case, some populations of those diagnosed (e.g. in China) are older and sicker than the general population and much less able to withstand aggressive treatment. After the SARS panic had subsided doctors reviewed the evidence, and it showed that these treatments were often ineffective, and all had serious side effects, such as persistent neurologic deficit, joint replacements, scarring, pain and liver disease. As well as higher mortality.
2. Introduction
The COVID-19 scare that emanated from Wuhan, China in December of 2019 is an epidemic of testing, as the graph below with test statistics from Austria shows. There is no proof that a virus is being detected by the test and, while there should be, there is absolutely no concern about whether there are a significant number of false positives on the test. What is being published in medical journals is not science, every paper has the goal of enhancing the panic by interpreting the data only in ways that benefit the viral theory, even when the data is confusing or contradictory. In other words, the medical papers are propaganda.

It is also an epidemic by definition. The definition, which assumes perfection from the test, does not have the safety valve that the definition of SARS did, thus the scare can go on until public health officials change the definition or realize that the test is not reliable. SARS, according to CDC, required a respiratory symptom; close contact with another SARS case or travel to a designated epidemic area; and a positive SARS test (or lack of antibodies believed to be protective) [48]. Once everyone had been quarantined, the second criterion was difficult to achieve outside of a hospital, and numbers plummeted.
What I learned from studying SARS, the previous big coronavirus scare, after the 2003 epidemic, was that nobody had proved a coronavirus existed, let alone was pathogenic. There was evidence against transmission, and afterwards, negative assessments of the extreme treatments that patients were subjected to, the nucleoside analog antiviral drug Ribavirin, high dose corticosteroids, invasive respiratory assistance, and sometimes oseltamivir (Tamiflu). This is documented in my draft book chapter (mostly complete) that you can find here:
http://theinfectiousmyth.com/book/SARS.pdf
3. Virus Existence
Scientists are detecting novel RNA in multiple patients with influenza or pneumonia-like conditions, and are assuming that the detection of RNA (which is believed to be wrapped in proteins to form an RNA virus, as coronaviruses are believed to be) is equivalent to isolation of the virus. It is not, and one of the groups of scientists was honest enough to admit this:
“we did not perform tests for detecting infectious virus in blood” [2]
But, despite this admission, earlier in the paper they repeatedly referred to the 41 cases (out of 59 similar cases) that tested positive for this RNA as, “41 patients… confirmed to be infected with 2019-nCoV.”
Another paper quietly admitted that:
“our study does not fulfill Koch’s postulates” [1]
Koch’s postulates, first stated by the great German bacteriologist Robert Koch in the late 1800s, are simple logic, and can be stated as:
- Purify the pathogen (e.g. virus) from many cases with a particular illness.
- Expose susceptible animals (obviously not humans) to the pathogen.
- Verify that the same illness is produced.
- Some add that you should also re-purify the pathogen, just to be sure that it really is creating the illness.
Famous virologist Thomas Rivers stated in a 1936 speech, “It is obvious that Koch’s postulates have not been satisfied in viral diseases”. That was a long time ago, but the problem continues. And Rivers’ guidance was considered important enough to be cited by papers claiming (falsely) that Koch’s Postulates had been met during the SARS era (2003). None of the papers referenced in this article have even attempted to purify the virus. And the word ‘isolation’ has been so debased by virologists it means nothing (e.g. adding impure materials to a cell culture and seeing cell death is ‘isolation’).
Reference [1] did publish electron micrographs, but it can clearly be seen in the lesser magnified photo, that the particles believed to be COVID-19 are not purified, as the quantity of material that is cellular is much greater. The paper notes that the photos are from “human airway epithelial cells”. Also consider that the photo included in the article will certainly be the “best” photo, i.e. the one with the greatest number of particles. Lab technicians may be encouraged to spend hours to look around to find the most photogenic image, the one that most looks like pure virus.
There is no way to tell that the RNA being used in the COVID-19 PCR test is found in those particles seen in the electron micrograph, because you cannot see what the contents are, they could be protein, RNA or DNA. There is thus no connection between the test, and the particles, and no proof that the particles are viral.
A similar situation was revealed in March 1997 concerning HIV, when two papers published in the same issue of the journal “Virology” revealed that the vast majority of what had previously been called “pure HIV” was impurities that were clearly not
HIV, and the mixture also included micro-vesicles that look very similar to HIV under an electron microscope, but are of cellular origin. [5][6]
4. Disease Definition
Infectious diseases always have a definition, but they are usually not publicized too widely because then they would be open to ridicule. They usually have a “suspect case” category based on symptoms and exposure, and a “confirmed” category that adds some kind of testing.
Reference [13] describes a suspect case definition for COVID-19, derived from WHO definitions for SARS and MERS (Middle East Respiratory Syndrome). This definition was in effect until January 18, 2020, and required all four of the following criteria:
- “Fever, with or without recorded temperature”. Note that there is no universal definition of fever, so this may just be the opinion of a physician or nurse. With SARS a fever was defined as 38C even though normal body temperature is considered to be 37C (98.6F).
- “Radiographic evidence of pneumonia”. This can occur without illness, as was seen in a 10 year old boy with no clinical symptoms [3]. He was diagnosed with pneumonia despite this.
- “Low or normal white-cell count or low lymphocyte count”. This is not really a criterion as every healthy person is included. This is also strange because people suffering from an infection normally have elevated white blood cell counts (although they may drop in people dying from an infection).
- One of the following three:
o “No reduction in symptoms after antimicrobial treatment for 3 days”. This is a standard indication of a ‘viral’pneumonia, i.e. one that does not resolve with antibiotics.
o “Epidemiologic link to the Huanan Seafood Wholesale Market”. This, and the next criterion, create the illusion of an infectious disease, as it prefers the diagnosis of connected cases.
o “Contact with other patients with similar symptoms”. On January 18th the last, three-part category was changed to:
• One of the following:
o “travel history to Wuhan”
o “direct contact with patients from Wuhan who had fever or
respiratory symptoms, within 14 days before illness onset”
The big problem is that, in contrast to the definition for SARS, a “confirmed case” of COVID-19 did not originally require the criteria for a suspect case to be met, but simply a positive RNA test. It did not require any symptoms or evidence of contact with previous cases, illustrating total faith in the PCR technology used in the test. The World Health Organization definition has the same flaw [15].
It was the fact that the SARS definition required both a reasonable possibility of contact with a previous case, and symptoms, that allowed the epidemic to burn out
Once everyone was quarantined, contact with an existing case was highly unlikely, testing stopped, and doctors could declare victory.
The Chinese eventually woke up and, around February 16th required confirmed cases to meet the requirements for a suspected case, as well as a positive test. They may have put this new definition into practice earlier because after a massive addition of almost 16,000 confirmed cases on February 12th, the number fell dramatically each day and, by February 18th was under 500 cases, and continued to stay low.
But other countries did not learn. Korea, Japan and Italy (and perhaps other countries) have started doing tests on people with no epidemiological link, encouraging people with the vague symptoms that are part of the definition to come to hospital to get checked, and obviously following up with anybody with a connection to them, most of whom will be asymptomatic. Consequently, in mid to late February, cases in those and other countries started to skyrocket.
A New Disease?
COVID-19 is described as a distinct new disease. But it clearly is not. There are no distinctive symptoms, for a start. Reference [2] showed that, among 41 early cases, the only symptoms found in more than half, were fever (98%) and cough (76%). 98% had CT Scan imaging showing problems in both lungs (although it is possible to have shadowing on a CT scan without symptoms). The high percentage of cases with fever and shadowing in both lungs is an artefact of the disease definition, fever and “radiographic evidence of pneumonia” are two of the diagnostic criteria for a probable case.
The low rate of people testing positive on the COVID-19 test is further evidence that there are no obvious symptoms. If there were recognizable symptoms, doctors should have a better than 3-5% chance of guessing who has the virus. While some of the people may have been tested, without symptoms, because they were on a flight or cruise, countries outside China are encouraging people with the non-specific symptoms of fever and cough to get tested, so increasingly people have symptoms of the flu or pneumonia, but are still testing negative in high numbers.
For example, as of March 9th, Korea had found 7,382 positive cases out of 179,160 people tested (4.1%) [20]. In Washington State, where they appear to be reluctant to test anyone, only 1 out of 27 tested by February 24th had tested positive (3.7%) [21]. Perhaps if they had tested all 438 who were then under quarantine, the epidemic would have exploded from 1 to about 16 cases (3.7% of 438). By March 9th, 1,246 tests had been performed in Washington with 136 found positive (11%). Obviously, in neither location can doctors recognize cases clinically.
5. Testing
Assuming, for a moment, the existence of a new coronavirus, what would a test tell us, at this stage? Or rather, what does it not tell us?
- Without purification and exposing animals to viral particles we do not know if the virus is pathogenic (disease causing). It could be an opportunistic infection (invades unhealthy people with weakened immune systems) or a passenger virus (that is carried along by risky behavior, such as eating an animal carrier of a virus).
- We don’t know the false positive rate of the test without validating a large number of positive tests by attempting to purify virus. Every positive test for which virus could not be purified would be a false positive, and every negative test for which virus could be purified would be a false negative. But the virus has not yet been purified, so test validation is impossible.
- If someone is sick there is no proof that any or all of their symptoms are due to the virus, even if it is present. Some people may be immune, some may have some symptoms caused by the virus, but others caused by the drugs they are given, by pre-existing health conditions, and so on.
- We don’t know if the people who test negative are infected or not, especially when they show up with similar symptoms. For example, in [2], out of 59 patients with similar symptoms, only 41 tested positive, but the researchers were clearly not sure whether the remaining 18 were truly uninfected. If they truly are not, they lend weight to COVID-19 not being the cause of any of the illnesses, as they had symptoms indistinguishable from the 41 positives. Testing at such an early stage of knowledge is incredibly dangerous. It spreads panic, it can put people on dangerous medications, other circumstances of their treatment can be physically and psychologically damaging (such as intubation and isolation, and even seeing all the doctors and nurses in special suits emphasizing how deathly sick you are).
False Negatives – Big Problem
According to an article in the South China Morning Post [23], Li Yan, head of the diagnostic center at the People’s Hospital of Wuhan University, noted on Chinese state TV that because of the multi-step process, an error at any stage could result in an incorrect outcome. This was echoed by reference [26] which noted the possibility of errors in the many steps from the time of specimen collection through processing. Wang Chen, president of the Chinese Academy of Medical Sciences, also on CCTV, said the accuracy is only 30 to 50 percent.
Wang Chen really means, however, that the test only ever produces false negatives, and never false positives. In a paper documenting a cluster of illness and positives tests in a family [3], this bias is clear, as most patients had more negative tests than positive tests, but were considered positive anyway. Patient 1 had 3/11 positive (27%), patient 2 had 5/11 (45%), patient 3 had all 18 negative, patient 4 had 4/14
(29%), patient 5 had 4/17 (24%) and patient 7 was the only with a majority positive (64%).
The only way to decide logically and scientifically is to have a gold standard for presence of the virus, which can only be purification and characterization (identification of the RNA and proteins). Since this has never been accomplished, doctors get to make decisions on the fly, biased towards treating patients as infected.
False Positives – Best Evidence
The first major attempt to define the false positive rate was in a paper describing a new test methodology, but it has a built-in conflict of interest [19]. Clearly, if the false positive rate was high, the authors’ aim to “develop and deploy robust diagnostic methodology for use in public health laboratory settings”, would have failed.
They did, however, do more than most. They took 297 samples of nasal and throat secretions from biobanks and tested them, only finding “weak initial reactivity” in four samples which, upon retesting, disappeared. The problem with this kind of analysis is that biobank samples may not have been obtained in the same way as samples from live people in an epidemic panic. The sampling was also not blinded, something that is necessary to eliminate the possibility of unconscious bias (a real problem in medicine). Furthermore, many samples in people believed to be infected are negative, and multiple samples are tested, as described for the family cluster paper. RNA is fragile if not stored carefully, and this would cause false negative results. No information on whether the samples were stored in a way designed to maintain RNA integrity was given.
Testing 297 samples could not even show that the false positive rate was under 1% with 99% certainty3, but because multiple samples are often taken in current COVID-19 test protocols, with any one positive sample over-ruling all the negatives, the false positive rate could be considerably higher, as the biobank samples were only tested once.
And, even if this test did have a false positive rate that was very low, it is not clear this particular test’s false positive rate can be extrapolated to any other test design.
Even a small false positive rate is critically important. A 99% accurate test would produce 110,000 false positives in a city of 11 million, like Wuhan. And if the number of positives in sampling is around 4% (which it appears to be from early statistics), then about 1 out of 4 positives would be false.
Finally, on March 5th 2020 some Chinese scientists dropped a bombshell. According to their analysis, based on reasonable assumptions for asymptomatic people
(e.g. contacts of other cases), “the false-positive rate of positive results was 80.33%”.[26] This is based on a mathematical analysis using reasonable
3 0.99297 ≈ 5%. A test with a 1% false positive rate would have a 5% chance of being used 297 times without a false positive being encountered. 0.985297 ≈ 1%.
assumptions for the actual prevalence of the virus, and the performance of the test. The best case, with the most optimistic assumptions, was still more than 40% false positives.4
Positive, Negative, Positive Again – Confusion
Some people have fully recovered from illness blamed on COVID-19, started to test negative, and then tested positive again. According to a news report [22] patients are not considered cured in China until they no longer have symptoms, have clear lungs, and have two negative COVID-19 tests. Despite this, 14% of discharged patients in Guangdong Province later tested positive, but with no relapse of symptoms. This is very difficult to explain if the test is for a virus, much easier to explain if the RNA that the test is looking for is not viral in origin. Later analysis showed similar results in Wuhan, with 5-10% declared to be “recovered” (negative tests after cessation of symptoms) later tested positive, often without symptoms [42]. Chinese scientists reported that 29 out of 610 patients at a hospital in Wuhan had 3-6 test results that flipped between Negative, Positive and ‘Dubious’ (undefined, but probably means a PCR cycle number between positive and negative) [52]. One patient, for example had three negative tests interspersed by two positive tests. Others had one test result in each of the three categories.
Confusing test results are listed in Appendix A.
Negative, Negative, Negative
A group of doctors in Marseille, France, working in a very experienced lab, that regularly does testing for respiratory viruses, reported testing 4,084 samples for COVID-19, using several systems approved for use in Europe, without a single positive [25]. This included 337 people returning from China who were tested twice, and 32 people referred because of suspected infection.
It is statistically improbable that this lab was just lucky to not get any COVID-19 cases, it is more likely that they used more stringent criteria, illustrating that the performance of not just test kits, but labs, with this new test, is completely unknown. Yet, a positive test remains unquestioned in every case.
Preserve the test
Overall, it seems that test results must be interpreted to preserve the coronavirus theory. No alternative interpretation is allowed. And when there is an inconsistency, it must be ignored or explained away, often invoking imaginary data. These situations are listed in Appendix A.
4 The abstract was eventually withdrawn, but without any explanation, indicating it was a political removal. The original Chinese language article was not retracted by the journal. This may be the first time ever that an abstract alone has been withdrawn.
Test Experience
A paper from Singapore by doctors and public health officials provides a revealing look at the inner guts of COVID-19 testing. Hidden away in the supplementary material of reference [24], where few people will see it, it exposes some important issues with tests:
- The test is not binary (negative/positive) and has an arbitrary cutoff.
- The quantity of RNA does not correlate with illness.
- If negative means uninfected and positive means infected, then people went from infected to uninfected and back again, sometimes several times.
- Results below the cutoff are not shown, and are treated as negative, but if PCR continued past the cutoff and was eventually positive, this would indicate presence of small quantities of the RNA which is supposedly unique to COVID-19 (i.e. infection).
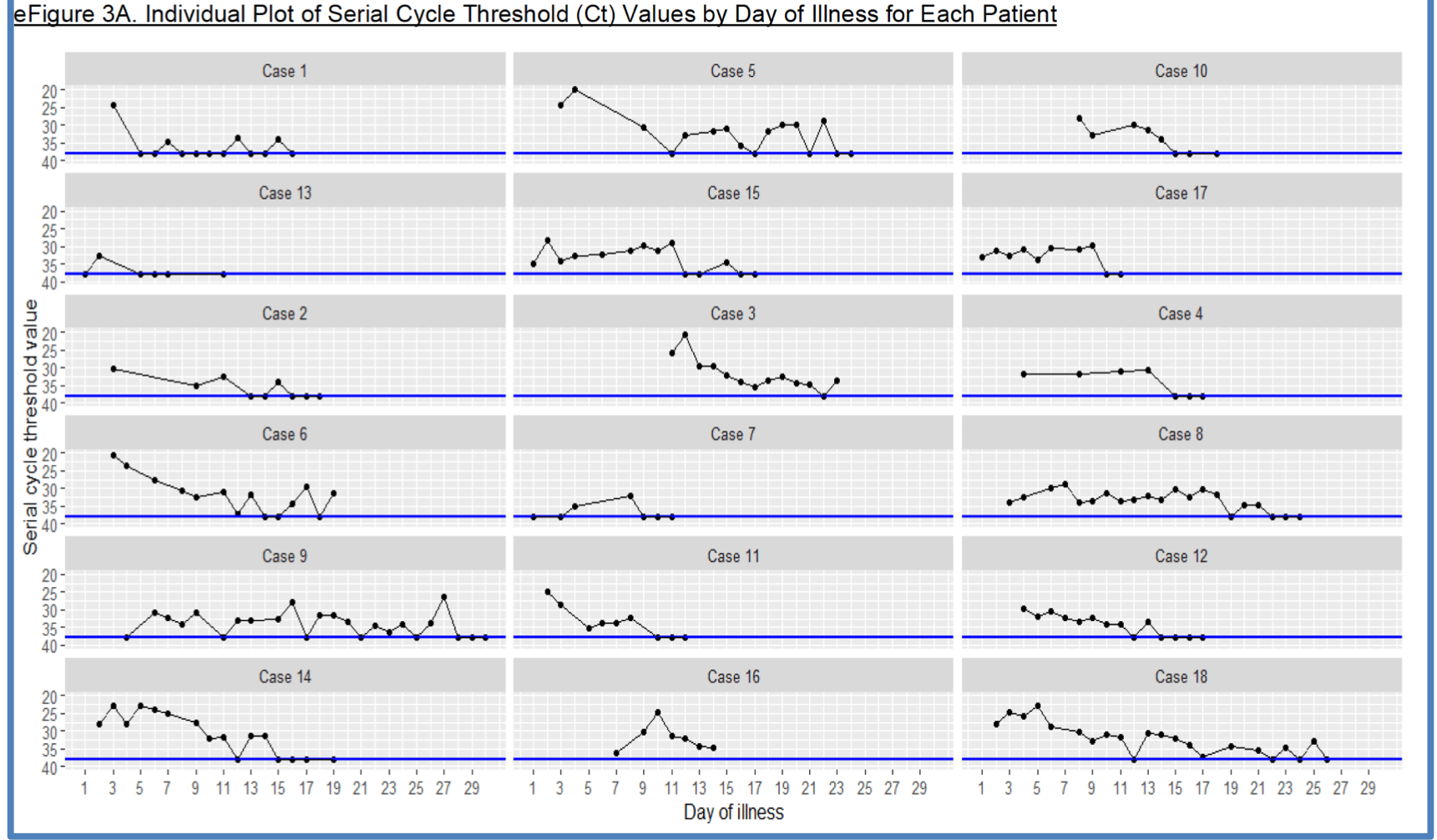
Before you read beyond the following figure, ask yourself why the first 6 graphs, shown deliberately out of numerical order, are separated. What are the visual differences between those 6 and the remainder? Do this right away so my interpretation does not bias your opinion.
The Test is Not Binary
Tests for infections are usually reported as positive or negative (sometimes ‘reactive’ and ‘unreactive’). One of the reasons for this is that, in many cases, multiple tests are required, and it is common to conclude that someone is infected even with some negative tests and that someone is uninfected even with some positive tests. The results of a complex multi-test algorithm are also usually reported as positive or negative, but interpreted by doctors and patients as infected or uninfected. The former could mean isolation, special medications, special precautions for health care workers and more.
But, in reality even individual tests are not binary, not positive or negative, but a range of numbers that are arbitrarily divided into positive on one side and negative on the other. Possibly there is a grey area that allows other factors, including the bias of the doctor or laboratory, to enter into the interpretation, or that will require further testing.
Understanding RT-PCR
Before we continue it is important to understand what RT-PCR, the test technology is. It is based on PCR (Polymerase Chain Reaction), a DNA manufacturing technique invented by the iconoclastic Kary Mullis, who received a Chemistry Nobel for it in 1993. It is one of the most important technologies invented since the rise of the biotech industry in the 1980s. Starting with one DNA strand, the strand is cleaved (split in two) and then complementary strands are allowed to grow, the same process that occurs in a cell during mitosis (cell division).
So far, not so impressive, but through the magic of doubling, if this process is repeated 10 times you will have about 1,000 identical strands of DNA. Twenty times, a million (220). Thirty times, a billion (230). Forty times, a trillion (240). Each round of doubling is referred to as a cycle.
To use (or abuse) PCR as a test, you assume that you are starting with an unknown number of strands and end up with an exponential multiple after n cycles. From the quantity of materials at termination the starting quantity can be estimated. A major problem with this is that because PCR is an exponential (doubling) process, errors also grow exponentially. In reality, the starting quantity is often not estimated, but the optical density, or another characteristic, of the growing pile of DNA, can be determined.
Another problem with many viruses, like coronaviruses, is that they are believed to be composed of RNA, but this can be solved by converting all RNA into DNA with the Reverse Transcriptase enzyme at the start of the process.
The technology, after these two adaptations, is known as RT-PCR (Reverse Transcriptase PCR).
Now you have the information necessary to understand the numbers from 20-40 on the vertical axis of the graphs above. These are the number of cycles. It implies that it always took at least 20 PCR cycles before any RNA could be detected, and they stopped after a maximum of 37 cycles. The blue line is at cycle 38, and the black dots do not mean RNA was detected after 38 cycles (as clarified in the paper), but that it wasn’t detected by 37 cycles, and so the process terminated. This “Serial Cycle Threshold (Ct)” was the arbitrary definition of a negative result by the authors of reference [24].
We can see that it was arbitrary, because in another paper, reference [13], the authors had two end points: 37 and 40. Anything less than 37 was considered positive and anything 40 or greater was defined as negative. The in-between values of 38 and 39 resulted in re-testing. Note that this paper would treat 37 as indeterminate but the Singapore paper would treat it as positive. In a review of 33 tests approved by the FDA under emergency conditions, where a PCR cycle number cutoff was recommended, it varied widely. One manufacturer each recommended 30 cycles, 31, 35, 36, 37, 38 and 39. 40 cycles was most popular, chosen by 12 manufacturers, and two recommended 43 and 45. The MIQE guidelines [61] recommend that data with 40 or more cycles should be discarded, and some feel that 35 is a better cutoff [57]. Among other problems, background fluorescence will build up and can produce a false positive with enough cycles.
Being arbitrary is not the only problem with the use of the cycle number. The values are not comparable between labs, and will vary within a lab, especially if even minor changes to the process are made (such as using clear plastic tubes instead of white plastic). In an audio interview, RT-PCR expert Professor Stephen Bustin stated that cycles should probably be limited to 35 [57]. The MIQE guidelines for use and reporting of RT-PCR, of which Bustin was a member, warn that “Cq [PCR cycle] values >=40 are suspect because of the implied low efficiency and generally should be reported”, specifically warning of the risk of false positives [61]. The examples above used 37 and 40 as the upper limit, and a workflow published by German hospital Charité Berlin, specified 45 cycles [58]. Tests from Altona Diagnostics and Vitassay, also recommend 45 cycles. A review of all the tests approved under emergency authorization by the US FDA showed that one test each recommended that positive be considered less than 30, 31, 35, 36, 37, 38, 39 cycles, 12 recommended less than 40, and one each recommended 43 and 45 [67].
RNA Quantity does not Correlate with Illness
Now to reveal the difference between the first six graphs and the remaining twelve!
Theoretically the PCR cycle number at which DNA is detectable tells us the relative quantity of RNA. Whatever initial amount was necessary to be detectable on the 20th cycle, 21 cycles would be doubly sensitive, and could detect about half as much, and 30 cycles about 1000th as much as 21. One could therefore expect sicker people to have more virus, and thus to have a lower cycle number on testing.
This is the reason the authors separated out the first six graphs from the remaining twelve. The first six were the people who were sick enough to require oxygen. But one can clearly see from the graph that the six sicker people did not have distinctly higher quantities of RNA, or any other consistent difference in their test graph.
In a survey of RNA-positive people in Guangdong, China, scientists examined the ‘viral load’ (quantity of RNA) and concluded that, “The viral load that was detected in the asymptomatic patient was similar to that in the symptomatic patients” [81].
Positive to Negative and Back Again
The majority of the 18 patients had a positive test, followed by a negative test, followed by a positive test. Some had this several times.
If a negative test means uninfected, then this is impossible. You cannot rid yourself of the virus, and then be re-infected the next day, and then infected the day after, and then become uninfected again. Or, if rapid re-infection is possible in a hospital setting, then the virus must be simply everywhere and fighting it is totally useless.
The simplest answer to this conundrum is that negative tests do not mean uninfected. But the corollary is that positive tests do not mean infected. Which would make the test worthless.
Results Below the Cutoff
The authors of reference [24] apparently programmed the PCR machine to stop after 37 cycles if no DNA had been detected. This means that we don’t have information on when or if the process would have terminated if it had been allowed to continue for many more cycles. More importantly, what would it mean if DNA was detected on cycle 38 or 40 or 80? If the RNA (complementary to the DNA used in PCR) is unique to the virus there is no other possible interpretation than that the person is infected. But it is possible that everyone would eventually detect enough material, which could only be interpreted as the corresponding RNA being endogenous (i.e. formed within the cells of the human body).
Given that several people bounced back from negative to positive again, one could argue that the cutoff should be more (or maybe less) than 37 cycles. But likely if this was done many more people might test positive, and even with a cutoff of, say, 40, going to negative and back again might still occur.
Symptoms Below the Cutoff
Another paper that contains a series of frequent tests, 1-5 days apart, for five European patients, showed that the PCR result (expressed in this case as estimated number of copies of RNA), went to undetectable (usually interpreted as negative or ‘uninfected’) 3 to 11 days before the cessation of symptoms, implying that the virus was causing illness when it wasn’t present [47]. Following is the graph of a patient with symptoms serious enough to justify prescription of the antiviral drug Remdesivir, who was COVID-19 negative (‘uninfected’) for 11 days before symptoms resolved. PCR testing is ultra-sensitive, so it is hard to sustain the idea that the virus was still present.

What is being looked for?
A review of 33 RT-PCR tests for COVID-19 approved under US FDA Emergency Use Authorizations showed a wide range of differences in what the tests were looking for and how they decided whether they had found it [67].
The tests look for a variety of different segments (‘genes’) of the presumed COVID- 19 genome, that only amounts to about 1% or less of the total genome, which is about 30,000 bases.
Perhaps the worst feature of the tests is how they decide whether the sample is positive if more than one segment is being looked for. Some tests look for only one, so it must be present for a positive. But tests that look for two segments are split between those that require both to be present and those that require either one for a positive. Some tests look for three segments but only require any two to be present, while one test insisted on all three.
Tests that allow a segment to be undetected raise the question of how it can be said that a virus was detected when an important part of it was missing.
As three doctors wrote in BMJ, “No test gives a 100% accurate result; tests need to be evaluated to determine their sensitivity and specificity, ideally by comparison with a ‘gold standard.’ The lack of such a clear-cut ‘gold-standard’ for covid-19 testing makes evaluation of test accuracy challenging.” The only gold-standard for an infectious disease is purification of the pathogen from those with positive tests, and inability to purify from people with negative tests [96].
6. Transmission
There is lots of evidence that the virus is not as transmissible as is being implied.
(January 2) “27 (66%) [of 41 early] patients had direct exposure to Huanan seafood market [i.e. about 1/3 did not]”. [2].
(January 1-20) “Of the 99 patients with 2019-nCoV pneumonia, 49 (49%) had a history of exposure to the Huanan seafood market.” [10] [i.e. 51% did not]
(January 1-January 22) A larger survey, including all the first 425 cases, showed that of those diagnosed January 1st or later, 72% had “No exposure to either market or person with respiratory symptoms”. [13]
“The symptom onset date of the first patient identified was Dec 1, 2019. None of his family members developed fever or any respiratory symptoms. No epidemiological link was found between the first patient and later cases.” [2]
(of the family cluster) “None of the family members had contacts with Wuhan markets or animals…They had no history of contact with animals, visits to markets including the Huanan seafood wholesale market in Wuhan, or eating game meat in restaurants.” [3]
(March 3) “Nearly 80% of patients with the new coronavirus in Japan have not passed on the infection to others regardless of the degree of their symptoms, a government panel of experts announced on March 2.” [43]
(May 6) The majority of recently hospitalized patients in New York are people who have followed the precaution of staying home. 66% were retired or unemployed and not commuting to work [80].
Transmission 1 – The Shenzhen Family Cluster
Reference [3] attempts to show the ease with which the virus could be transmitted in a family that travelled from Shenzhen, near Hong Kong, to Wuhan in December, and then back again about a week later.
Two grandparents (patients 1 and 2), the daughter and son-in-law (patients 3 and 4), a 10-year old grandson and a 7-year old granddaughter (patients 5 and 6) flew to Wuhan on December 29th. On the first day, the grandmother (1) and her daughter (3) visited a baby boy with pneumonia, known as Relative 1, in a hospital in Wuhan (the hospital is not named, but the implication is that this child had this new disease). Outside of this they mingled with four other local relatives, of which two had also spent extensive time in the hospital. Notably the infant’s symptoms resolved one or two days after the visit, and he returned home.
On day four of the visit (January 1st), the son-in-law, who had not gone to the hospital got sick. On this basis, they declared that COVID-19 had a very short incubation time, and that people were almost immediately infectious. There’s no evidence for this, except nothing else can support their hypothesis that the
hospitalized baby had COVID-19, infected Patients 1 (grandmother) and 3 (daughter), one of which then infected the son-in-law (Patient 4). All in four days.
Then, like dominoes, the other visitors got sick, the daughter one day after her husband (Jan 2), the grandmother the next day (Jan 3), and then the grandfather and Relatives 2, 3, 4 and 5 (Jan 4). The family appeared to have a history of being frequently ill. In this case symptoms were mostly fever, cough and weakness.
On January 4th the whole family returned to Shenzhen. Note that the grandchildren, patients 5 and 6, had no symptoms during their time in Wuhan, or after returning home.
On January 9th, the grandparents and their daughter went to a clinic in Shenzhen, and the next day the grandparents visited the big hospital (University of Hong Kong- Shenzhen Hospital) for tests. The daughter followed one day later (January 10th).
The grandparents had significant pre-existing health conditions, such as having been treated for brain cancer (grandmother) and hypertension (both). In Wuhan they both suffered from fever, dry cough, weakness, and later were found to have various lab abnormalities. They were genuinely sick.
Concern that they were infected with COVID-19 is probably the reason why the rest of the family were brought in over the next few days for testing. The daughter and son-in-law were still sick (diarrhea, congestion, sore throat, chest pain) but by then had a normal body temperature (actually lower than 37C). They did have some lung opacities on a CT scan, so were diagnosed with pneumonia despite the normal temperature.
The grandson had been a bad boy (patient 5) and had refused to wear a mask in Wuhan, so the parents insisted he get a CT scan. Despite the complete lack of symptoms, he also had lung opacities, and so was also diagnosed with pneumonia, albeit completely asymptomatic.
The granddaughter was a good girl (patient 6), and had worn a mask, and so nobody was surprised that she was not only asymptomatic, but also did not have lung abnormalities.
All six patients (apparently including patient 6 who was healthy in all ways) were tested using the new RNA test. Not surprisingly, the grandparents tested positive on nose swabs and serum samples. The son-in-law tested positive on nose and throat samples. But the daughter, Patient 3, despite doing 18 tests, more than anyone else, stubbornly tested negative on each one. But, showing shocking bias, the authors concluded, “she was still regarded as an infected case because she was strongly epidemiologically linked to the Wuhan hospital exposure and radiologically showing multifocal ground-glass lung opacities.” Another indication of bias was the omission of test results for Patient 6, who also tested similarly tested negative every time (but based on only four samples, according to personal correspondence from the authors). In this case the bias was clearly to classify her as uninfected.
The bad grandson (patient 5) also tested positive on nose, throat and sputum samples, despite having no symptoms of illness.
Additionally, there was a relative who did not travel to Wuhan (Patient 7), who got sick with back pain and weakness four days after everyone returned to Shenzhen and, when she was tested, she also tested positive for RNA (nose, throat and sputum).
Several of the relatives who lived in Wuhan also got sick afterwards, but no COVID- 19 test information was provided in this paper.
No consideration was given to other causes for illness, such as exposure to food contaminated by chemicals, food that was prepared in anticipation of their visit, that was left out too long, or in unsanitary conditions. The purpose of reference [3] appears to have been to prove that the putative COVID-19 is infectious, not to try to disprove it (which is what good scientists should do). Note that the relatives visited each other a lot over a few days, that was indeed the purpose of the trip, and one can guess that they ate more than usual, ate richer and more exotic foods (but not exotic animals) and perhaps drank more than usual. But none of this was investigated.
Transmission 2 – The German Connection
Reference [9] attempts to connect the illness of some Germans, one of whom met with a Chinese woman, who afterwards was diagnosed positive on the RNA test.
The sequence of events started between January 20th and 22nd when a woman from Shanghai and a local German were in meetings together. Both were healthy at the time5. The woman flew back to China on January 22nd and started to feel sick on the flight home. The German also got sick (sore throat, chills, muscle pain, fever, cough), late on the 24th, and did not return to work until the 27th. By coincidence, this was the same day that the Shanghai woman informed the German company that she had been sick and had tested positive for COVID-19 RNA. By this time the German man had recovered without any special medicines or interventions, but he tested positive, and so did three other colleagues who had contact with him, or the Shanghai woman, or both. It is logical that everyone who had any contact with them was tested, and likely no employees who did not have contact were tested. The paper does not say how many tested negative, and whether any of those testing negative had similar symptoms.
The article claims that all four Germans had symptoms starting on the 24th, 26th, or 27th, but what those symptoms were is not detailed for the three not in the meeting with the Chinese woman. The article does note that, “so far, none of the four confirmed patients show signs of severe clinical illness”.
If the purpose of the paper was to support the idea that this illness is transmissible, it is important to accept the four positive tests on Germans as true positives, despite the fact that none of them had “severe clinical illness”. This, however, calls into question the severity of the illness, and why heroic and dangerous medical measures are needed. Because the Germans did not find out about their positive RNA test until after their period of symptoms, they probably only had to suffer
5 A later letter from the Robert Koch Institute noted that the authors of the article had not interviewed the woman, and she had actually been suffering from fatigue and muscle pain.
quarantine, and not antiviral drugs, steroids or invasive respiratory assistance, which might have happened if they had shown up at an emergency department with symptoms and had been diagnosed with COVID-19 at the same time.
An alternative explanation is that COVID-19 is deadly, but that these four Germans represent four false positive tests. If this is the case, the usefulness of the test must be questioned.
Note that the fact that all the people with positive tests and symptoms had contact is not surprising if testing was limited to people who had contact.
Transmission 3 – Illinois Couple
A paper in Lancet made a big deal about the presumed first case of person-to-person contact in the USA, from a woman who had visited Wuhan in December 2019, to her husband, who had stayed in the United States. She got sick after returning, and later both her and her husband, who had not travelled to Wuhan, tested positive for COVID-19 [31]. Whether he had symptoms or not was impossible to tell because he had chronic obstructive pulmonary disease, so had a cough and difficulty breathing all the time. What is more interesting is that authorities identified 372 contacts of this couple, and “were able to assess exposure risk and actively monitor symptoms for 347”. Not one of these people had an emergency room visit with respiratory symptoms within 14 days of contact with the couple. 43 did have some symptoms that could have been COVID-19, and became “Persons Under Investigation” (PUIs). 26 had had exposures to the couple classified as “medium risk or greater”. But despite the presence of symptoms, contact with the couple, and close monitoring, not one tested positive for COVID-19.
Transmission 4 – Chinese Heart Patient [88]
A young woman in Guangzhou China with congenital heart disease was hospitalized for a long time without suspicion that she was COVID-19 RNA-positive. By the time she tested positive, 455 people had had contact with her, including hospital staff, other patients, and family members. All contacts were traced, and despite 8 having respiratory symptoms, all 455 tested RNA-negative.
Transmission 5 – Diamond Princess [33]
The Diamond Princess cruise ship was a perfect laboratory for watching a highly infectious pathogen in action. The first person who tested positive had symptoms before boarding the ship on January 20th. It was not until February 1st that they tested positive, and February 3rd when passengers were confined to their quarters, in some cases with someone who tested positive. Passengers had interactions with the crew, e.g. to obtain meals. Despite this, the rate of transmission was only 16.7%, meaning that 83.3% remained negative. Since almost half those who tested positive had no symptoms it was not possible to avoid contact with positive persons based on observing symptoms, and it meant that 92% emerged from quarantine without having experienced symptoms due to COVID-19.
Transmission 6 – Magical
Numerous newspaper articles have noted cases outside China (where individual cases were still newsworthy) that had no known contact with another case, or travel to an endemic region (notably Wuhan). These are documented in Appendix A.
Proving Transmission
It is impossible, in most cases, to prove that someone did have contact with another COVID-19 case, even if they did travel to Wuhan and visit the Huanan market. In the best case it will be possible to show that someone was in the vicinity of someone who tested positive earlier, but that does not constitute proof that they were exposed to the virus, let alone that it was that person who infected them. In most cases, even if someone was in Wuhan, there will be no evidence that a person was in contact with another victim.
Fundamentally, this belief that it is contact that causes positive tests is necessary to preserve the infectious paradigm. Therefore, the slightest evidence of an association between an old case and a new case (such as having been in the same city at the same time) is taken as proof of transmission, when it is obviously not.
7. Treatment
Treatment for the putative novel coronavirus, COVID-19, is following the same pattern as for SARS. Apart from standard treatment for respiratory conditions, there is a tendency towards providing oxygen to patients more aggressively (e.g. intubation), the use of high dose corticosteroids (e.g. methylprednisolone) and a variety of antiviral medications.
SARS Experience
This did not work out well for SARS. As a report, commissioned by a WHO expert panel after SARS was over, said,
“Despite an extensive literature reporting on SARS treatments, it was not possible to determine whether treatments benefited patients during the SARS outbreak. Some may have been harmful…Of patients treated with ribavirin, 49/138 to 67/110 (36%–61%) developed haemolytic anaemia [breakdown of red blood cells], a recognised complication with this drug, although it is not possible to rule out the possibility that SARS-CoV infection caused the haemolytic anaemia, as there is no control group. One study noted that over 29% of SARS patients had some degree of liver dysfunction indicated by ALT levels higher than normal, and the number of patients with this complication increased to over 75% after ribavirin treatment…In the Chinese literature, we found 14 reports in which steroids were used. Twelve studies were inconclusive and two showed possible harm. One study reported diabetes onset associated with methylprednisolone treatment. Another study (an uncontrolled, retrospective study of 40 SARS patients) reported avascular necrosis and osteoporosis among corticosteroid-treated SARS patients [which resulted in many joint replacements, particularly in Hong Kong]” [7].
Drugs for COVID-19
For SARS the antiviral drug ribavirin was dominant, but for COVID-19, a wider variety of antivirals were proposed at the beginning of the panic, and now it has expanded beyond just antivirals to anti-malaria and rheumatology drugs. The choice of drugs is a shot in the dark as, “There are no proven therapies for the prevention or treatment of COVID-19. All agents have the possibility of associated harm” [40]:
- Flu drug oseltamivir (Tamiflu) [2]. Use was described as “empirical”, based on intuition, not science. Usage in China was also reported in [10]. A JAMA review states that there is “no role in the management of COVID-19 once influenza has been excluded” [53].
- A JAMA review notes that another influenza drug, Umifenovir (Arbidol) is approved in Russia and China. Non-randomized, observational data showed a significantly lower death rate, and randomized trials are underway in China [53].
- AIDS drug combination Kaletra, composed of protease inhibitors Lopinavir and Ritonavir, has been fairly widely used. A Chinese hospital noted that the
choice was because the drug was “already available in the designated hospital” [2]. Usage in China was also reported in [10] and in Singapore in [24]. On March 18th Chinese researchers published an article declaring their clinical trial a failure, noting that the drug was, “not associated with clinical improvement or mortality in seriously ill patients with Covid-19 different from that associated with standard care alone.” [38]. This was echoed by a JAMA review that suggests, “a limited role for lopinavir/ritonavir”, and noted significant drug-drug interactions at dosages suggested [53].
- Nelfinavir is another AIDS protease inhibitor, mentioned in [28].
- Cytomegalovirus drug Ganciclovir (Cytovene) was also reported in China by [10].
- Early in February the Chinese government announced a trial of Gilead’s Ebola antiviral Remdesivir, on the basis that it, “may have helped alleviate the symptoms of a 35-year-old male” diagnosed with COVID-19 infection in the US [15]. The drug was going to be trialed on 270 people, although it is not clear whether there will be a placebo or comparison group. A Chinese chemistry professor, Jiang Xuefeng, warned, “No random, controlled, or blank samples were used in [its previous use in one American man]…The effectiveness of remdesivir cannot be determined by this single case…It can take years to fully understand the pharmacological and toxicological side effects of new drugs”[15]. Reference [28] admits that, “randomized and controlled trials are still needed to determine the safety and efficacy of remdesivir.” Some of those trials are happening at 12 centres in Italy [35]. By April, 2020, Gilead had enrolled 4,000 people in two trials, and one of the sites, University of Chicago Medicine, with about 3% of total patients, announced positive results, but a press report included a significant caveat, “The lack of a control arm in the study could make interpreting the results more challenging” [56]. Notwithstanding this, Gilead share prices quickly rose 16%. But on April 23rd Gilead stock crashed back down when the Chinese reported that slightly more of the Remdesivir patients died (14% vs 13% on ‘standard care’) and 11.6% had to stop the drug early versus 5.1% in the control group [74]. On April 16th Gilead changed the primary end point of one trial from an 8 point scale (1=dead through 8=healthy) to “time to recovery”, which ignores patients who died [78].
- A Japanese hospital used the anti-influenza medication Avigan (Favipiravir) on one patient, it was given to 70 patients in Shenzhen, China [30], and is being tested in Italy as well [35].
- A review of treatments in China, published mid-February, also revived the use of Ribavirin despite admitting lack of effectiveness and “significant toxicity”. But perhaps, they hypothesized, it would be useful combined with other drugs [28]. A JAMA review notes its hematologic and liver toxicity, and no discernable benefit with the coronavirus MERS [53].
- There has been much excitement about the anti-malaria drugs chloroquine (aka Nivaquine, Plaquenil), and the less toxic hydroxy-chloroquine. Neurological side effects, sometimes permanent, are the most worrying side
effect of this family of drugs. A JAMA review of drugs indicated that, “no high- quality evidence exists for the efficacy”, the only data from China is a news report. The drug is reported as relatively safe, but there is a warning about side effects in less than 10% of people, “including QTc prolongation, hypoglycemia, neuropsychiatric effects, and retinopathy…and the potential for arrythmias” [53]. Shortly after the JAMA review was published, a clinical trial of chloroquine in 81 people in Brazil had to be halted when patients developed irregular heart rates [54]. A researcher in the trial is quoted as saying that, “the high dosage that the Chinese were using is very toxic and kills more patients.” 6
- Related drug hydroxychloroquine has been heavily promoted, including by US President Trump. A German pulmonologist has claimed that the modified G6PD gene found in many Africans makes hydroxychloroquine “very dangerous” to them [77]. A New York state study found an elevated risk of death with hydroxychloroquine combined with azithromycin, but it was not statistically significant, and the study design was observational, not randomized, further reducing confidence in the result. There was no evidence of benefit [82]. A Chinese study of high dose hydroxychloroquine (800-1200mg) similarly found no benefit in preventing disease progression (it was actually slightly higher with the drug) and 10% of patients had diarrhea, and 2/70 had unspecified ‘serious adverse events’. The group without hydroxychloroquine did not experience these problems [84].
- Russia promoted a related malaria drug, Mefloquine (Lariam), even though this has a well-documented risk of serious neurological side effects, often permanent. https://www.rt.com/russia/484364-russian-drug-treatment-covid19/
- Tocilizumab (Actemra), a rheumatoid arthritis drug from Roche, is also being tested in Italy [35]. It blocks immune system protein interleukin-6 (IL-6) and is considered immunosuppressive.
- Siltuximab, a similar rheumatoid arthritis drug, is also under consideration.
- Sarilumab (Kevzara) from Regeneron and Sanofi, another IL-6 inhibitor, is also entering a clinical trial. https://www.healio.com/rheumatology/rheumatoid- arthritis/news/online/%7B1957db6e-f7a2-4e5d-939e-d4b5964b2dd3%7D/sarilumab- enters-clinical-trial-for-covid-19-spotlighting-key-role-for-il-6
- Interferon-β has shown activity against MERS, but combined with other drugs. In conclusion, a JAMA review states that, “Given conflicting in vitro and animal data and the absence of clinical trials, the use of interferons to treat SARSCoV- 2 cannot currently be recommended” [53].
- Interferon-α is also being used by the Chinese and Cubans, but very little information about safety and effectiveness is available.
- A JAMA review recommends further study of antihelminthic (anti-intestinal worm) drug Nitazoxanide on the basis of broad antiviral activity (in the test tube) and a “relatively favorable” safety profile [53]. 6 A multi-hospital study on Chloroquine and Hydroxychloroquine has been removed because it was retracted.
- Pancreatitis drug Camostate mesylate has some test tube evidence in favor of future study [53].
- There is a small amount of evidence in favor of further research on Favipivir (T-705) on the basis of a study comparing it with Arbidol for COVID-19, although the adverse effects that can be expected at the higher dosages believed necessary are unknown [53].
- There are reports of the use of corticosteroids with COVID-19. For example, 27% of the first 2,003 Italians whose deaths were blamed on COVID-19 had received corticosteroids [32]. These drugs were widely used during SARS, but afterwards it was found that they were associated with an increased risk of psychosis, diabetes and osteonecrosis. Based on this experience, plus similar experiences with influenza and MERS, also blamed on a coronavirus, a report in Lancet recommended against their use in COVID-19 [73]. These drugs are sometimes described as “experimental”, but that is a misnomer, and disguises the fact that they are not used in the context of science. It is clearly not science when there is often no placebo, no blinding, and no randomization. It is likely that sicker patients will be prescribed untested drugs, if they have a health decline it will be blamed on the virus, and nobody could know what would have happened if they had received standard medical treatment for their symptoms. At best there will be a comparison between two unproven drugs. If the patient survives it will likely be considered a success, and is worth millions, or more, in public relations to the drug company.
Drug Usage
93% of 41 confirmed Chinese COVID-19 cases in [2] received Oseltamivir, and future use of Kaletra was planned. 75 of 99 patients, also in China, received unspecified antivirals [10]. 58% of 29,692 COVID-19 positive people who died in Italy had been prescribed (unspecified) antivirals [32].
Invasive Ventilation7
Patients with respiratory illnesses like pneumonia often have difficulty getting enough oxygen into their blood (oxygenation). This is because there is a reduced amount of lung tissue (alveoli) available for gas exchange, perhaps because it is disabled by the collection of fluids and pus or inflammation. When a patient is found to have low oxygen levels or signs of respiratory distress (such as rapid, shallow breathing sweating or grogginess) providing more oxygen is required. There are increasing levels of oxygenation support that can be given, with increasing risk:
- Tubes to the nose (cannulas) that deliver air richer in oxygen.
- Oxygen masks can provide higher levels of oxygen.
- Intubation, inserting a tube down the throat to the lungs.
The last method, which is known as invasive ventilation, has significantly greater risks. After SARS an analysis of data in Hong Kong compared one hospital that started patients with non-invasive ventilation to 13 that immediately went to intubation for SARS [36]. Despite this one hospital receiving significantly sicker patients, their death rate was more than four times lower, and there were no instances of transmission of SARS to health care workers.
One problem with intubation is the cluster of issues known as VALI – Ventilator Association Lung Injury [45]. Another is Ventilator Associated Pneumonia (VAP). While most patients already have pneumonia, this problem could introduce new pathogens. Risk factors relevant to COVID-19 patients include chronic disease, previous antibiotic therapy and hospitalization for over 5 days [39].
Invasive ventilation can also be traumatic, with patients experiencing, “unreal experiences…often associated with intense fear” [40]. Care by nurses and relatives can reduce this fear, but when relatives are barred from the bedside, and nurses are cloaked in personal protective gear, there may be no comforting face or hand- holding available.
It appears that concerns about invasive ventilation from the SARS era are being ignored. In the UK, an analysis of 6,718 patients showed that 67% were intubated within 24 hours of admission [37]. One reason is that the UK government is strongly advising sick people to stay home and self-isolate (“Do not leave home if you or someone you live with has either: a high temperature a new, continuous cough”) and to not go to an emergency room until their symptoms worsen. This could lead to people with early, easily treated pneumonia, waiting several days, at which point their pneumonia is much more advanced and may require intubation. This is not to advocate that people should go to an ER for any sniffle or slight fever, but the pendulum may have swung too far the other way, with the minority of people whose cold or flu symptoms do not resolve in two or three days waiting too long to get help.
A second reason for intubation is the fear of infection of health care workers or other patients with non-invasive ventilation, despite that fear being unfounded with SARS. In the UK, advice is based on this fear, therefore, “a low threshold should be applied to early intubation and mechanical ventilation” [49]. In Australia and New Zealand, “Early intubation should be considered to prevent the additional risk to staff of emergency intubation and to avoid prolonged use of high flow nasal oxygen or non-invasive ventilation” [50]. And a review of experiences in Italy stated that, “Invasive ventilation is associated with reduced aerosolisation and is thus safer for staff and other patients”, but also admitted that, “it might also be associated with hypoxia, haemodynamic failure and cardiac arrest during tracheal intubation” [51].
In the United States, ventilation is associated with higher payments from the government. Although they vary by region, they are approximately $13,000 for a regular COVID-19 patient and $39,000 for an intubated patient [75].
Problems with intubation can occur due to improper insertion of the tubes causing internal damage (perhaps because the patient is not completely sedated), and due to secretions from the mouth, upper airways or even stomach entering the lungs. The procedure is harder on patients with a weaker constitution due to age or pre-
existing health conditions. And problems may be exacerbated by the use of other powerful drugs, such as those being proposed and used for coronavirus treatment. Sufficient trained staff are also needed to constantly monitor and care for the immobilized patients, and to be able to properly extubate them (remove the tube) if oxygen levels go back up again.
If damage from invasive ventilation occurs, it will be almost impossible to differentiate it from worsening of the underlying lung problem, so the deterioration may be ascribed to the wrong cause. But it has been associated with shockingly high death rates. One patient survey from China reported that 31 out of 32 (97%) intubated patients die [60]. A New York patient survey reported that 320 out of 5700 COVID-19 patients were intubated. Even among the younger group, 18-65, the death rate was 76%, and among those over 65, the same shocking 97% as in China [70].
Increasingly, it is being found that advanced non-invasive alternatives to intubation are safer and often eliminate the need to intubate. A JAMA paper showed that the use of facemasks reduced the risk of death, compared to standard oxygen therapy, by about 20%, and the use of a special helmet, by about 60%. Helmets reduced the need for intubation by about three-quarters, face masks by about one-quarter and even high-flow nasal oxygen by about the same amount [97].
Treatment experience
We do not have much precise documentation of experiences with the antiviral drugs, this tends to come out after an epidemic is over, when doctors have time to go through the copious records that will be taken, and see if they can determine whether the treatments had any impact on the markers of the disease or on the health of the patient. Since it is almost certain that there was no control, it will be impossible to distinguish between a patient who recovered on their own despite the treatment, and one who was saved by the treatment. However, useful information on adverse events and disease markers can be obtained.
The first report of treatment experience that I am aware of came from Singapore [24]. They reported on 18 patients, of which only five received antiviral medications, chosen from six sickest patients, who required supplemental oxygen.
The doctors used the AIDS drugs Lopinavir and Ritonavir, often marketed as the combination pill Kaletra. For two of the patients they reported a reduction of oxygen requirements within 3 days, and for two they started to get negative coronavirus tests (not the same two). So far, so good, although it is impossible to claim this is due to the drugs, and it was only a minority of the patients.
The bad news is that two patients, “deteriorated and experienced progressive respiratory failure while receiving lopinavir/ritonavir, with 1 requiring invasive mechanical ventilation”. And these two patients continued to produce positive coronavirus tests. Furthermore 3 out of 5 patients “developed abnormal liver function test results” and 4 out of 5, “developed nausea, vomiting, and/or diarrhea”.
In total, only one of the five was able to complete the planned 14-day course of antiviral drugs.
It is of course not possible to prove that the drugs produced the side effects or worsening of health that is seen, as a control is impossible during an epidemic panic. However, when the condition of the patients includes known side effects of the drugs prescribed, it is reasonable to infer that they are caused by the drugs.
Conclusions
In the following section on Treatment, it is shown that coronavirus positive patients who die are generally older and sicker than the general population. This means that they are less able to withstand aggressive treatment. It is known that the treatments have side effects, that these can be quite severe, but it is not yet known if any of them have benefits.
8. Mortality
There are four main questions to ask about mortality:
- Are the number of cases significant in the context of normal mortality?
- Is the death rate of cases higher than other similar diseases, such as influenza?
- Who is dying?
- Are there reasons for death other than a novel coronavirus?
Number of Cases
Many people are convinced that COVID-19 is a severe problem by the large number of deaths it is causing. For example, at the time of writing, Worldometer was reporting about 164,000 deaths from COVID-19, to date, representing about 0.002% of the global population.
One reason this number is misleading is because it is a cumulative number, and not a weekly number. If we divide by the 8 weeks that, at the time of writing, the panic had been in western countries, it amounts to about 20,500 deaths per week, over the entire globe.
Another reason the number is misleading is that few people have any idea how many people die on a weekly basis in their country. For example, in the United States, a country of about 325 million, there were about 2.8 million deaths in 2017 according to the CDC, or about 54,000 per week. So normal deaths in the United States per week are between two and three times larger than global deaths due to the coronavirus.
Death Rate of Cases
While ordinary people might have been panicking due to the sheer scale of the number of deaths, medical and scientific people were panicking over the high death rate. The death rate is simply the number of deaths from coronavirus divided by the total number of cases. A problem is that the number of cases who have been discovered may be vastly less than the real number of cases, because asymptomatic people are much less likely to be tested, and this dramatically increases the apparent death rate. Secondly, people may be recorded as coronavirus deaths when it was not the main cause of death, and this also dramatically increases the apparent cause of death.
As an example, take a town that has 100 confirmed coronavirus cases and 10 deaths. The death rate is 10% which is 100 times more than influenza (0.1%). But a recent study, using an antibody survey, found that there were 50-85 times more people positive in Santa Clara County, hard hit by the COVID-19 panic, than confirmed cases would indicated. Then a 10% death rate would drop to between 0.2% and 0.1%.
But what if only 12% of people registered as coronavirus deaths actually died from the coronavirus death, as the scientific advisor to Italy’s Minister of Health, stated in an interview with Britain’s Daily Telegraph [62]? Then a 10% death rate declines to under 1%. The United States also has a policy of recording most deaths of
coronavirus-positive people as deaths from the coronavirus, even if the death was obviously from one of their pre-existing health conditions combined with old age [62]. In Belgium, all deaths at retirements homes are classified as COVID-19 although only 5% have tested positive for the virus [71]. Similarly, 55 deaths at a nursing home in Brooklyn, USA, were classified as COVID-19 despite the fact that, “not a single resident has been able to get tested for the virus to this day” [72].
If we multiply the number of coronavirus cases by 50 while taking 12% of the deaths as truly from coronavirus, then our 10% death rate drops to 0.02%, which is significantly less than influenza.
Who is Dying?
Coronavirus patients are generally older and weaker than the general population. For example, “The average age of the patients was 55.5 years, including 67 men and 32 women” [10]. Only about 12% of the Chinese population are 55 or over [11]. In a later study [13], the median age was 59, and only about 10% of Chinese are this age or older. In the last of three time periods of this study, January 12th through 22nd, the median age had crept up to 61.
The patients also were likely to have pre-existing health conditions. For example, “50 (51%) patients had chronic diseases, including cardiovascular and cerebrovascular diseases, endocrine system disease, digestive system disease, respiratory system disease, malignant tumour, and nervous system disease” [10].
These characteristics are exacerbated for those who died, they are even older and unhealthier than coronavirus patients in general. In Italy, the average age of coronavirus patients was just over 60, but the average age of 29,692 deaths was 80. Only 1.1% of the deaths were in people under 50, and 0.2% under 40. All those under 40 for which information was available had “serious pre-existing pathologies”.
96% of cases for which information was available had serious at least one pre- existing health condition (68% had hypertension, and smaller quantities had diabetes, other heart conditions, recent cancer, kidney failure, COPD, stroke, dementia and chronic liver disease) that could have explained the deaths. 60% had over three conditions, 21% had two and 15% had one.[32].
A UK report of 3,912 deaths of coronavirus positive people found similar characteristics of the deceased. The largest proportion of deaths were in those aged 85-89, with only one death in people under 20. 91% had at least one pre-existing health condition, and the average number was 2.7. These included ischaemic heart disease; Alzheimers and dementia; Chronic lower respiratory diseases; Influenza and pneumonia; and Diabetes [55].
A report from New York showed that 88% of 5,700 COVID-19 patients had more than one pre-existing health condition, several of which are often associated with difficulty breathing (morbid obesity, asthma, COPD, etc). The death rate was highest in those 80 and older, 54%, and dropped dramatically with reduced age. Only 32%
of those in their 70s died, 16% in their 60s, 12% in their 50s, 6% in their 40s, 4% in their 20s and 30s. Nobody under 20 died [70].
A New England Journal of Medicine report with 8,910 patients from 169 hospitals worldwide showed that age over 65, coronary artery disease, cardiac arrhythmia and current smoking each approximately doubled the risk of death when hospitalized for COVID-19, and Chronic Obstructive Pulmonary Disease almost tripled the risk [79].8
A German report on 10 autopsies of COVID-19-RNA-positive people found an average age of 79 and between 1 and 6 pre-existing co-morbidities (average of 3) [85].
Non-Viral Causes of Death
It is generally believed that any surplus deaths seen since February could only have been caused by COVID-19, but there are actually several ways in which our panic could have caused death. Unfortunately, due to the evolving situation, and dearth of the appropriate information, quantifying these deaths is currently impossible:
- Aggressive medical treatment.
- Early Palliative Treatment
- Isolation.
- Delaying going to hospital.
- Consequences of home confinement.
- Consequences of germphobia.
- Air pollution.
- Diet and nutrition. Aggressive medical treatment
The Treatment section above describes the special medical treatments that are only given to people who test coronavirus positive or who, in some cases, are believed to be coronavirus infected based on symptoms. Both intubation and drug treatments have side effects that can be fatal, although it is not possible at present to quantify the number of deaths being cause.
Early Palliative Treatment
Guidance from the Spanish Society for Palliative Care (SECPAL) recommends that in the cases where very sick patients with difficulty breathing are not accepted into an ICU, the hospital or residence should immediately move to palliative care. This includes starting the patient on the opioid Morphine, the anti-psychotic Haloperidol (Haldol, to reduce nausea from morphine), sometimes Buscapine (Scopolamine) to reduce nasal and mouth secretions, and Midazolam, a benzodiazepine, if more sedation is needed. This appears to be tantamount to euthanasia as sedatives and narcotics can cause respiratory depression [90].
8 Deleted because of questions about all data from the Surgisphere database. 32
A statement approved by the European Board of the Association for Geriatric Palliative Medicine seems to similarly define palliative care for COVID patients as a drug induced coma. Respiratory distress requires morphine. Acute respiratory distress adds Midazolam. Anxiety requires the benzodiazepine sedative Lorazepam and Midazolam. Even cough requires morphine and codeine. Pain requires morphine. Delirium requires Haloperidol and Midazolam. Most symptoms will be treated by heavily sedating the patient [91].
Isolation and Neglect
COVID-19 patients are generally isolated from the outside world, not able to see visitors, and not seeing staff as humans because they are hidden behind layers of personal protective gear. The literature on the benefits of visitation to patients is too vast to cite here, but visitors can help patients understand what medical staff are saying and proposing to do, provide emotional comfort, relieve boredom, and make the patient continue to believe that their life is worth the struggle to continue. Visitors also are likely to notice dramatic declines in physical or mental functioning, and ask questions about medications and care. If the only people seen are in protective gear that further emphasizes the dire circumstances, and the small likelihood of recovery.
In a paper studying Italian data, the authors obviously thought that greater social- connectedness would increase the number of COVID-19 cases among older people, due to increased opportunities for transmission. But in places where old people tended to live with families there were fewer cases among those 80 and older, and more cases where they tended to live alone or in nursing homes, “Paradoxically, the results are opposite of what was previously reported. The pandemic was more severe in regions with higher family fragmentation and increased availability of residential health facilities”. They note that the nursing homes quickly banned visitors, so it is likely something about the isolated old people in nursing homes that was the cause of more deaths [93].
Canadian soldiers were called in to assist with 5 care homes in Ontario, Canada, and were so shocked at what they saw, that they wrote a detailed letter documenting their concerns. Just some of the deficiencies included: unsanitary catheterization, liquid (parenteral) feeding and wound care changes; inadequate or inaccessible wound care supplies; leaving patients lying in one position for days or weeks; sedation of patients who just miss their families; no psychosocial support for lonely patients; forceful and aggressive feeding and patient movement; leaving food in a sleeping patient’s mouth; not assisting patients who need help eating; not sitting patients up properly to receive food, liquids or medications; poor documentation of medication usage; cockroaches and flies; rotten food left by a patient’s bedside; inadequate feeding and especially hydration; patient falls not properly documented or examined; no procedure for patients to receive supplies from their families, such as reading material, snacks and personal care products [94].
Delaying treatment
In the United Kingdom the government put up posters that have messages similar to this: “If you or anyone in your household has a high temperature or a new and continuous cough – even if it’s mild, (A) Everyone in your household must stay at home for 14 days and keep away from others; (B) DO NOT go to your GP, hospital or pharmacy; (C) Only call NHS 111 if you can’t get online or your symptoms worsen.” This is a very clear message that sick people must stay home. In most cases their symptoms probably resolve, but if they progress to pneumonia the affected person may still delay going to the hospital, and when they do arrive their pneumonia may be much further advanced than under normal circumstances.
Patients may also decide for themselves that they do not want to go to an Emergency Room because of the perception that it will be full of people infected with COVID-19, and a certain way to pick up the infection.
In New York, people in cardiac arrest whose hearts cannot be restarted at the scene will not be driven to the hospital for further resuscitation attempts, according to the New York Post on April 2nd due to fear that hospitals are overwhelmed with coronavirus patients (nypost.com/2020/04/02/coronavirus-nyc-emts-stop-taking-cardiac- arrest-patients-to-hospitals). By contrast, in Birmingham, in the UK, paramedics are told to pick up the patient but not to start chest compressions or ventilation in the ambulance, but to wait until they arrive at the hospital, due to fear of contamination of the ambulance with COVID-19 (https://www.bmj.com/content/368/bmj.m1282).
Consequences of home confinement
In Canada, the Justice Centre for Constitutional Freedoms, a legal action group, wrote to Prime Minister Trudeau and provincial premiers, asking their governments to quantify various harms from home confinement and other restrictions on movement and association, including deaths from:
- Increased suicide rates, e.g. due to unemployment, bankruptcy or hopeless poverty due to loss of employment or closure of a small business. For example, in one county of Tennessee, in one week, there were more suicides (9) than in the entire State for the duration of the epidemic panic [86].
- Deaths from alcoholism and drug abuse, exacerbated by loss of employment, loss of social interactions and isolation. The Wall Street Journal reported in late May that prescriptions for addictive anti-anxiety medications and sleeping pills have risen significantly (10-34%) since the beginning of the COVID-19 panic [92].
- Domestic abuse from forcing partners to stay in close quarters for extended periods of time, when one of the partners is already abusive.
- Deaths of elderly, infirm people due to lack of visitors to observe their deteriorating physical and mental condition.
- Deaths from cancellations of elective surgeries or from inability to access hospital services. An organization that is a “leading provider of data to NHS [National Health Service] trusts” (Edge Health) warned on April 25th that
there might already be 2,000 medical deaths per week from the non-COVID impacts of the coronavirus panic, such as among stroke, heart attack and diabetes patients who can no longer access needed services [76].
• Future deaths from increased poor health in children (e.g. diabetes) who have few opportunities for exercise or fresh air.
A study in JAMA, although it did not investigate mortality, showed a shocking rise in psychological distress in US adults, comparing a survey of 1,468 in April 2020 to a similar survey in 2018. Psychological distress rose from 3.7% in 18-29 year olds to 24%, from 7.9% among adults earning less than $35,000 per year to 19.3%, and from 4.4% among Hispanic adults to 18.3% [95].
Consequences of germphobia
Modern societies have long had a fear of microbes, with many people seeing them only as a source of sickness, despite many foods containing bacteria or fungi, such as cheese, yogurt, kefir, miso soup, kombucha, pickles, olives, kimchi, sauerkraut (if not pasteurized), tempeh and more.
The coronavirus panic has led to vastly increased (although probably futile) efforts at disinfection of any surfaces that people could come in contact with. This may well cause long term problems, such as the development of cancer, but in the short term it has already been associated with a sharp increase in calls to US poison control centers, according to the CDC [65].
Air pollution
Many people noted that both Wuhan and Lombardy Italy, two hotspots for coronavirus deaths, also suffered from heavy air pollution. Now there is some scientific support for this. Harvard University scientists found that an increase of 1 microgram of fine particulates per cubic meter was associated with an 8% increase9 in COVID-19 deaths [68]. An Italian study concluded that, “people living in an area with high levels of pollutant are more prone to develop chronic respiratory conditions and suitable to any infective agent. Moreover, a prolonged exposure to air pollution leads to a chronic inflammatory stimulus, even in young and healthy subjects. We conclude that the high level of pollution in Northern Italy should be considered an additional co-factor of the high level of lethality recorded in that area” [69]. Air pollution may leave people more vulnerable, both to any new health challenges, and to aggressive medical treatment.
Diet and nutrition
A study comparing COVID-19 patients in ICU to patients in a regular ward found that Vitamin D Insufficiency was present in 11/13 (85%) of the former but only 4/7 (57%) of the latter. 7/20 (35%) of ICU patients had critically low levels. All COVID- 19 ICU patients less than 75 years old had Vitamin D deficiency. The authors note that Vitamin D deficiency is much more common among people over 60 and black-
skinned people, and that hydroxychloroquine raises plasma Vitamin D levels. Note that this is a small study, so can only be considered preliminary [83].
The Lockdown?
In an interesting analysis of the peak of COVID-19 mortality, in places where it rose far above historical averages, John Pospichal shows that this always occurred immediately after the lockdowns commenced. Reasons for this are unclear, but the vast majority of people were old, with pre-existing health conditions and many were residing in care homes. One of the first edicts of all lockdowns was banning visitors to these homes. Any change in treatment of those who died in these homes with visitors absent needs to be investigated [89].
9. Conclusions
The coronavirus panic is just that, an irrational panic, based on an unproven RNA test, that has never been connected to a virus. And which won’t be connected to a virus unless the virus is purified. Furthermore, even if the test can detect a novel virus the presence of a virus is not proof that it is the cause of the severe symptoms that some people who test positive experience (but not all who test positive). Finally, even if the test can detect a virus, and it is dangerous, we do not know what the rate of false positives is. And even a 1% false positive rate could produce 100,000 false positive results just in a city the size of Wuhan and could mean that a significant fraction of the positive test results being found are false positives.
The use of powerful drugs because doctors are convinced that they have a particularly potent virus on their hands, especially in older people, with pre-existing health conditions, is likely to lead to many deaths. As with SARS.
There is very little science happening. There is a rush to explain everything that is happening in a way that does not question the viral paradigm, does not question the meaningfulness of test results, and that promotes the use of untested antiviral drugs. And, given enough time there will be a vaccine developed and, for some of the traumatized countries, it may become mandatory, even if developed after the epidemic has disappeared, so that proving that it reduces the risk of developing a positive test will be impossible.
10. References
- Zhu N et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020 Jan 14. https://www.nejm.org/doi/full/10.1056/NEJMoa2001017
- Huang C et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020 Jan 24. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30183-5/fulltext
- Chan J F-W et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020 Jan 24. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30154-9/fulltext
- Rivers TM. Viruses and Koch’s Postulates. J Bacteriol. 1937 Jan; 33(1): 1-12. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC545348/
- Gluschankof P et al. Cell membrane vesicles are a major contaminant of gradient-enriched human immunodeficiency virus type-1 preparations. Virology. 1997 Mar 31; 230(1): 125-133. http://davidcrowe.ca/SciHealthEnv/papers/277-Microvesicles-Gluschankof.pdf
- Bess JW et al. Microvesicles Are a Source of Contaminating Cellular Proteins Found in Purified HIV-1 Preparations. Virology. 1997 Mar 31; 230(1): 134-44. http://davidcrowe.ca/SciHealthEnv/papers/278- Microvesicles-Bess.pdf
- Stockman LJ et al. SARS: Systematic Review of Treatment Effects. PLoS Med. 2006 Sep 12; 3(9). http://davidcrowe.ca/SciHealthEnv/papers/5253-SARS-Treatment-Effects.pdf
- Fourth case of novel coronavirus confirmed in Canada. Globe & Mail. 2020 Jan 31. https://www.theglobeandmail.com/canada/article-fourth-case-of-novel-coronavirus-confirmed-in-canada/
- Rothe C et al. Transmission of 2019-nCoV Infection from an Asymptomatic Contact in Germany. N Engl J Med. 2020 Jan 30. https://www.nejm.org/doi/full/10.1056/NEJMc2001468
- Chen N et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020 Jan 30. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30211-7/fulltext
- Population pyramid for China. https://www.populationpyramid.net/china/
- Kim C-R. Three Japanese evacuees from Wuhan test positive for virus, two had no symptoms. Reuters. 2020 Jan 29. https://www.reuters.com/article/uk-china-health-japan/three-japanese-returnees-from- wuhan-test-positive-for-coronavirus-nhk-idUKKBN1ZT02K
- Li Q. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus–Infected Pneumonia. N Engl J Med. 2020 Jan 29. https://www.nejm.org/doi/full/10.1056/NEJMoa2001316
- Singapore confirms first cases of local coronavirus transmission: What we know about the 6 new cases, Health News & Top Stories. The Straits Times. 2020 Feb 4. https://www.straitstimes.com/singapore/health/singapore-confirms-first-cases-of-local-coronavirus- transmission-what-we-know-about
- Haiyun W. China To Begin Testing Ebola Drug on Coronavirus Patients. Sixth Tone. 2020 Feb 3. https://www.sixthtone.com/news/1005155/china-to-begin-testing-ebola-drug-on-coronavirus-patients
- Global Surveillance for human infection with novel coronavirus (2019-nCoV): Interim guidance. WHO. 2020 Jan 31. https://www.who.int/publications-detail/global-surveillance-for-human-infection-with-novel- coronavirus-(2019-ncov)
- Diagnosis and treatment: COVID-19 prevention and control. China CDC. 2020 Feb 16. http://www.chinacdc.cn/en/COVID19/202002/P020200217499154038416.pdf
- Countries/areas with reported cases of Coronavirus Disease-2019 (COVID-19). CHP. 2020 Feb 22, 27. [This is a regularly updated page, and the PDF file will change] https://www.chp.gov.hk/files/pdf/statistics_of_the_cases_novel_coronavirus_infection_en.pdf
- Corman VM et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020 Jan; 25(3). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6988269/
- Korea Coronavirus Cases. KCDC. 2020 Feb 25-27 [accessed]. https://www.cdc.go.kr/board/board.es?mid=a30402000000&bid=0030
38
- Novel Coronavirus Outbreak 2020. Washington State Department of Health. 2020 Feb 24 [accessed]. https://www.doh.wa.gov/Emergencies/Coronavirus
- Koop F. A startling number of coronavirus patients get reinfected. ZME Science. 2020 Feb 26. https://www.zmescience.com/science/a-startling-number-of-coronavirus-patients-get-reinfected/
- Feng C et al. Race to diagnose coronavirus patients constrained by shortage of reliable detection kits. South China Morning Post. 2020 Feb 11. https://www.scmp.com/tech/science-research/article/3049858/race- diagnose-treat-coronavirus-patients-constrained-shortage
- Young BE et al. Epidemiologic Features and Clinical Course of Patients Infected With SARS-CoV-2 in Singapore. JAMA. 2020 Mar 3. https://jamanetwork.com/journals/jama/fullarticle/2762688
- Letter to the editor: Plenty of coronaviruses but no SARS-CoV-2. Eurosurveillance. 2020 Feb 27. https://www.eurosurveillance.org/content/10.2807/1560- 7917.ES.2020.25.8.2000171?fbclid=IwAR1yaTgICfc15rO6mkI90pBb45j1EnT87KA5p9gcfnixqSciJWsFeQb4j5I
- Zhuang GH et al. [Potential false-positive rate among the ‘asymptomatic infected individuals’ in close contacts of COVID-19 patients]. Zhonghua Liu Xing Bing Xue Za Zhi. 2020 Mar 05; 41(4): 485-488. Chinese full text: http://html.rhhz.net/zhlxbx/017.htm English translation:http://theinfectiousmyth.com/articles/ZhuangFalsePositives.pdf
- Confirman nuevo caso de contagio del coronavirus causante de Covid-19 [New case of coronavirus confrmed]. Granma. 2020 Mar 12. http://www.granma.cu/cuba-covid-19/2020-03-12/covid-12-03-2020-21- 03-51
- Zhang L et al. Potential interventions for novel coronavirus in China: A systematic review. J Med Virol. 2020 Feb 13. https://onlinelibrary.wiley.com/doi/full/10.1002/jmv.25707
- Lei J et al. CT Imaging of the 2019 Novel Coronavirus (2019-nCoV) Pneumonia. Radiology. 2020 Jan 31. https://pubs.rsna.org/doi/10.1148/radiol.2020200236
- Zhou C et al. Coronavirus: experimental treatments give hope as China death toll hits 1,523. South China Morning Post. 2020 Feb 15. https://www.scmp.com/news/china/society/article/3050773/coronavirus- hubei-reports-2420-new-cases-and-139-additional
- Ghinai I et al. First known person-to-person transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the USA. Lancet. 2020 Mar 13. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30607-3/fulltext
- Characteristics of SARS-CoV-2 patients dying in Italy. ISS. 2020 May 14. https://www.epicentro.iss.it/en/coronavirus/bollettino/Report-COVID-2019_14_may_2020.pdf
- Russell TW et al. Estimating the infection and case fatality ratio for COVID-19 using age-adjusted data from the outbreak on the Diamond Princess cruise ship. medrxiv. 2020 Mar 5. https://www.medrxiv.org/content/10.1101/2020.03.05.20031773v2.full.pdf
- Grasselli G et al. Critical Care Utilization for the COVID-19 Outbreak in Lombardy, Italy: Early Experience and Forecast During an Emergency Response. JAMA. 2020 Mar 13. https://jamanetwork.com/journals/jama/fullarticle/2763188
- Cuppini L. Covid-19 al via i farmaci che fanno sperare [COVID-19, the drugs we have been hoping for]. Corriere della Sera. 2020 Mar 24. https://www.corriere.it/salute/malattie_infettive/20_marzo_24/covid-19- farmaci-che-fanno-sperare-sono-oggetto-studi-clinici-8ae11f80-6d45-11ea-ba71-0c6303b9bf2d.shtml
- Yam LY et al. Non-invasive versus invasive mechanical ventilation for respiratory failure in severe acute respiratory syndrome. Chin Med J (Engl). 2005 Sep 5; 118(17): 1413-21. http://davidcrowe.ca/SciHealthEnv/papers/5164-Ventilation-SARS.pdf
- Report on COVID-19 in critical care. ICNARC. 2020 Apr 17. https://www.icnarc.org/DataServices/Attachments/Download/c5a62b13-6486-ea11-9125-00505601089b
[This replaced an earlier version, now removed from the internet, that was referenced until version 8.1]
- Cao B et al. A Trial of Lopinavir-Ritonavir in Adults Hospitalized with Severe Covid-19. N Engl J Med. 2020 Mar 18. https://www.nejm.org/doi/full/10.1056/NEJMoa2001282
- Wu D et al. Risk Factors of Ventilator-Associated Pneumonia in Critically III Patients. Front Pharmacol. 2019 May 9; 10: 482. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6521332/
- Clinical Care (Coronavirus). BCCDC. 2020 Mar [accessed]. http://www.bccdc.ca/health- professionals/clinical-resources/covid-19-care/clinical-care
39
- Granberg A et al. Acute confusion and unreal experiences in intensive care patients in relation to the ICU syndrome. Part II. Intensive Crit Care Nurs. 1999 Feb; 15(1): 19-33.
- Feng E et al. Some Recovered Coronavirus Patients In Wuhan Are Testing Positive Again. NPR Goats and Soda. 2020 Mar 27. https://www.npr.org/sections/goatsandsoda/2020/03/27/822407626/mystery-in- wuhan-recovered-coronavirus-patients-test-negative-then-positive
- Nearly 80% of coronavirus patients in Japan have not infected others: experts. The Mainichi. 2020 Mar 3. https://mainichi.jp/english/articles/20200303/p2a/00m/0na/012000c?fbclid=IwAR1mh4PzJDQyzW3b8Kc4V 86mXq9VqB0j_muBkXjGd03SIDeWnjUGSkH3-uU
- Khan FA. Personal correspondence with FA Khan, MD. 2020 Mar.
- Slutsky A et al. Ventilator-Induced Lung Injury Review. PulmCCM. 2013 Dec 7. https://pulmccm.org/review- articles/ventilator-induced-lung-injury-review-nejm/
- Anzahl Tests und positiver Ergebnisse [Tests Performed and Positive Results]. Trending Topics. 2020 Apr 2. https://www.trendingtopics.at/corona-faelle-oesterreich/
- Clinical and virological data of the first cases of COVID-19 in Europe: a case series. Lancet. 2020 Mar 27. https://www.sciencedirect.com/science/article/pii/S1473309920302000
- Updated interim surveillance case definition for Severe Acute Respiratory Syndrome (SARS) – United States, April 29, 2003. MMWR. 2003 Apr 29; 52. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5217a5.htm
- Information about 2019-nCoV for UK Critical Care Departments. Intensive Care Society. 2020 Feb 11. https://www.ics.ac.uk/ICS/ICS/Pdfs/News/Official_2019-nCoV__critical_care_FAQ_and_advice.aspx
- Brewster DJ et al. Consensus statement: Safe Airway Society principles of airway management and tracheal intubation specific to the COVID-19 adult patient group. The Medical Journal of Australia. 2020 Mar 16. https://www.mja.com.au/journal/2020/consensus-statement-safe-airway-society-principles-airway- management-and-tracheal
- Sorbello M et al. The Italian coronavirus disease 2019 outbreak: recommendations from clinical practice. Anaesthesia. 2020 Mar 27. https://onlinelibrary.wiley.com/doi/full/10.1111/anae.15049
- Li Y et al. Stability issues of RT-PCR testing of SARS-CoV-2 for hospitalized patients clinically diagnosed with COVID-19. J Med Virol. 2020 Mar 26. https://onlinelibrary.wiley.com/doi/full/10.1002/jmv.25786
- Sanders JM et al. Pharmacologic Treatments for Coronavirus Disease 2019 (COVID-19): A Review. JAMA. 2020 Apr 13. https://jamanetwork.com/journals/jama/fullarticle/2764727
- Thomas K et al. Small Chloroquine Study Halted Over Risk of Fatal Heart Complications. NY Times. 2020 Apr 12. https://www.nytimes.com/2020/04/12/health/chloroquine-coronavirus-trump.html
- Deaths involving COVID-19, England and Wales. Office for National Statistics. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deat hsinvolvingcovid19englandandwales/ deathsoccurringinmarch2020
- Feuerstein A et al. Early peek at data on Gilead coronavirus drug suggests patients are responding to treatment. STAT. 2020 Apr 16. https://www.statnews.com/2020/04/16/early-peek-at-data-on-gilead- coronavirus-drug-suggests-patients-are-responding-to-treatment/
- Crowe D. Episode 251: Stephen Bustin on Challenges with RT-PCR. The Infectious Myth. 2020 Apr 14; 251. https://infectiousmyth.podbean.com/e/the-infectious-myth-stephen-bustin-on-challenges-with-rt-pcr/
- Corman V et al. Diagnostic detection of 2019-nCoV by real-time RT-PCR. Charité Virology. 2020 Jan 17. http://davidcrowe.ca/SciHealthEnv/papers/12715-RT-PCR_Coronavirus.pdf
- RECOVERY Trial. University of Oxford. 2020 Apr 18 [accessed]. https://www.recoverytrial.net/
- Zhou F et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 Mar 11. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30566-3/fulltext
- Bustin SA et al. The MIQE guidelines: minimum information for publication of quantitative real-time PCR experiments. Clin Chem. 2009 Apr; 55(4): 611-22. https://academic.oup.com/clinchem/article/55/4/611/5631762
- Newey S. Why have so many coronavirus patients died in Italy? The Telegraph. 2020 Mar 23. https://www.msn.com/en-au/news/world/why-have-so-many-coronavirus-patients-died-in-italy/ar- BB11qA65
40
- New ICD code introduced for COVID-19 deaths. NVSS. 2020 Mar 24. https://www.cdc.gov/nchs/data/nvss/coronavirus/Alert-2-New-ICD-code-introduced-for-COVID-19- deaths.pdf
- Trudeau and Premiers questioned about consequences to human health and lives from government- imposed lockdowns. JCCF. 2020 Apr 14. https://mailchi.mp/jccf/trudeau-and-premiers-questioned-about- consequences-to-human-health-and-lives-from-government-imposed-lockdowns
- Chang A et al. Cleaning and Disinfectant Chemical Exposures and Temporal Associations with COVID-19 — National Poison Data System, United States, January 1, 2020–March 31, 2020. MMWR. 2020 Apr 20; 69. https://www.cdc.gov/mmwr/volumes/69/wr/mm6916e1.htm
- Not in use.
- Emergency Use Authorizations for COVID-19 Tests. FDA. 2020 Apr 19. https://www.fda.gov/medical- devices/emergency-situations-medical-devices/emergency-use-authorizations
- Wu X et al. Exposure to air pollution and COVID-19 mortality in the United States. medRxiv. 2020 Apr 5. https://www.medrxiv.org/content/10.1101/2020.04.05.20054502v1
- Conticini E et al. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ Pollut. 2020 Apr 4; 114465. https://www.sciencedirect.com/science/article/pii/S0269749120320601
- Richardson S et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA. 2020 Apr 22. https://jamanetwork.com/journals/jama/fullarticle/2765184
- ¿Por qué Bélgica es el país con más muertos por millón de habitantes? [Why is Belgium the country with the most deaths per million inhabitants?]. as. 2020 Apr 17. https://as.com/diarioas/2020/04/17/actualidad/1587139438_994913.html
- ’Under Siege’: Overwhelmed Brooklyn Care Home Tolls 55 Dead. US News & World Report. 2020 Apr 20. https://www.usnews.com/news/politics/articles/2020-04-20/under-siege-overwhelmed-brooklyn-care- home-tolls-55-dead
- Russell CD et al. Clinical evidence does not support corticosteroid treatment for 2019-nCoV lung injury. Lancet. 2020 02 15; 395(10223): 473-475. https://www.thelancet.com/journals/lancet/article/PIIS0140- 6736(20)30317-2/fulltext
- Boseley S. First trial for potential Covid-19 drug shows it has no effect. The Guardian. 2020 Apr 23. https://www.theguardian.com/world/2020/apr/23/high-hopes-drug-for-covid-19-treatment-failed-in-full- trial
- Rogers M. Fact check: Hospitals get paid more if patients listed as COVID-19, on ventilators. USA TODAY. 2020 Apr 24. https://www.usatoday.com/story/news/factcheck/2020/04/24/fact-check-medicare- hospitals-paid-more-covid-19-patients-coronavirus/3000638001/
- Nuki P. Two new waves of deaths are about to break over the NHS, new analysis warns. The Telegraph. 2020 Apr 25. https://www.telegraph.co.uk/global-health/science-and-disease/two-new-waves-deaths- break-nhs-new-analysis-warns/
- Wodarg W. Covid-19 – a case for medical detectives. multipolar. 2020 May 2. https://multipolar- magazin.de/artikel/covid-19-a-case-for-medical-detectives
- Adaptive COVID-19 Treatment Trial (ACTT). ClinicalTrials.gov. 2020 May 4 [accessed]. https://clinicaltrials.gov/ct2/show/NCT04280705
- Removed due to integrity problems with Surgisphere data
- Slattery D. ’Shocking’: 66% of new coronavirus patients in N.Y. stayed home: Cuomo. NY Daily News. 2020 May 6. https://www.nydailynews.com/coronavirus/ny-coronavirus-cuomo-coronavirus-stats- 20200506-eyqui4b5lfdn7g6cqswkf6otly-story.html
- Zou L et al. SARS-CoV-2 Viral Load in Upper Respiratory Specimens of Infected Patients. N Engl J Med. 2020 Mar 19; 382(12): 1177-1179. https://www.nejm.org/doi/full/10.1056/NEJMc2001737
- Rosenberg ES et al. Association of Treatment with Hydroxychloroquine or Azithromycin with In-Hospital Mortality in Patients With COVID-19 in New York State. JAMA. 2020 May 11. https://jamanetwork.com/journals/jama/fullarticle/2766117
- Lau FH et al. Vitamin D Insufficiency is Prevalent in Severe COVID-19. medRxiv. 2020 Apr 24. https://www.medrxiv.org/content/10.1101/2020.04.24.20075838v1
41
- Tang W et al. Hydroxychloroquine in patients with mainly mild to moderate coronavirus disease 2019: open label, randomised controlled trial. BMJ. 2020 May 14; 369: m1849. https://www.bmj.com/content/369/bmj.m1849.long
- Schaller T et al. Postmortem Examination of Patients With COVID-19. JAMA. 2020 May 21. https://jamanetwork.com/journals/jama/fullarticle/2766557
- Mastrangelo D. Suicides outpacing coronavirus deaths in Tennessee, data says. Washington Examiner. 2020 May 22. https://www.washingtonexaminer.com/news/suicides-outpacing-coronavirus-deaths-in- tennessee-data-says
- Removed due to integrity problems with Surgisphere data
- Gao M et al. A study on infectivity of asymptomatic SARS-CoV-2 carriers. Respir Med. 2020 May 13; 106026. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7219423/
- Pospichal J. Questions for the lockdown apologists. Medium. 2020 May 24. https://medium.com/@JohnPospichal/questions-for-lockdown-apologists-32a9bbf2e247
- Orientaciones sobre el control sintomático de enfermos graves afectados por la enfermedad COVID 19 y que requieran atención paliativa o se encuentren próximos al final de la vida [Guidance over the control of symptoms to those gravely ill from COVID-19 and who require palliative care or are near the end of their life]. SECPAL. 2020 Mar 22.https://www.secpal.com/Documentos/Blog/2020_03_23%20FIN%20DE%20VIDA%20Y%20COVID%2019%20 _1.%20Documento%20para%20profesionales_1.pdf
- Kunz R et al. COVID-19 pandemic: palliative care for elderly and frail patients at home and in residential and nursing homes. Swiss Medical Weekly. 2020 Mar 24. https://smw.ch/article/doi/smw.2020.20235
- Petersen A. More People Are Taking Drugs for Anxiety and Insomnia, and Doctors Are Worried. WSJ.
2020 May 25. https://www.wsj.com/articles/more-people-are-taking-drugs-for-anxiety-and-insomnia-and- doctors-are-worried-11590411600 - Liotta G et al. Is social connectedness a risk factor for the spreading of COVID-19 among older adults? The Italian paradox. PLoS One. 2020; 15(5): e0233329. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0233329
- Mialkowski CJJ. Letter to Headquarters, Fourth Canadian Division Joint Task Force (Central). Personal Correspondence. 2020 May 19. http://www.documentcloud.org/documents/6928480-OP-LASER-JTFC- Observations-in-LTCF-in-On.html
- McGinty EE et al. Psychological Distress and Loneliness Reported by US Adults in 2018 and April 2020. JAMA. 2020 Jun 3. https://jamanetwork.com/journals/jama/fullarticle/2766941
- Watson J et al. Interpreting a covid-19 test result. BMJ. 2020 May 12; 369: m1808. https://www.bmj.com/content/369/bmj.m1808.long
- Ferreyro BL et al. Association of Noninvasive Oxygenation Strategies With All-Cause Mortality in Adults With Acute Hypoxemic Respiratory Failure: A Systematic Review and Meta-analysis. JAMA. 2020 Jun 04. https://jamanetwork.com/journals/jama/fullarticle/2767025
42
Appendix A Confusing Test Results
Some test results simply do not make sense if the test accurate reflects an infection that comes, making someone positive, and then goes, returning the person to negative. Often, when ‘impossible’ test results occur, authorities tie themselves in knots trying to explain the test without questioning the accuracy of the RT-PCR RNA test for COVID-19 or the viral paradigm.
- (Jan 24) As mentioned above, in Reference [3] the daughter, important in the chain of transmission of a family, was interpreted as a false negative. Alternatively it could have been concluded that this woman did not have the coronavirus, but that would have badly damaged the family transmission story, and left open other reasons for the cluster of illnesses (and CT scan abnormalities).
- (Jan 24) Also in Reference [3] the grandson tested positive without any symptoms at all, except lung abnormalities on a CT scan. This allowed them to declare him as ill (asymptomatic pneumonia). But he could have been an asymptomatic case or a false positive.
- (Jan 29) Out of 206 Japanese evacuated from Wuhan, only three tested positive, and two were found to have “no symptoms”. Instead of considering them false positives, they are considered infected and possibly infectious.[12]
- (Jan 30) The four Germans [9] could be seen as showing that the RNA test produces false positives or that the illness produced by the virus is often not severe. But it will be interpreted as neither by dogmatic promoters of the coronavirus theory, it simply will not be mentioned now that the main message, that the virus is infectious, is bolstered by the evidence.
- (Jan 31) A woman who returned from China to her Canadian university with illness, first tested negative, and then positive. This was interpreted as indicating that she had very little virus in her body at the time of the first test, and that the test was not sensitive enough. However, PCR testing is extraordinarily sensitive, and if she had so little virus, how was it that she had symptoms? An alternative explanation is that she became positive on the test in Canada, perhaps because this virus is actually quite common, or because the test is not for a virus, but is just measuring RNA created by the human body in response to disease conditions.[8]
- (Feb 2) An 80 year old Hong Kong man tested positive after hospital admission due to a fever, but his only recent trip to mainland China was a brief visit to Shenzhen, just outside Hong Kong (over 1000km from Wuhan by car). He had no contact with other cases, markets with live animals or wild animals. https://news.rthk.hk/rthk/en/component/k2/1506121-20200202.htm
- (Feb 4) Of 6 positive cases in Singapore reported in [14], the first had a sore throat and cough, but no pneumonia, the second and third had undescribed symptoms, and the last three had no symptoms.
43
- (Feb 11) A sick woman in Wuhan tested negative on her first test, after days of illness, but positive on the second. https://www.scmp.com/tech/science- research/article/3049858/race-diagnose-treat-coronavirus-patients-constrained-shortage
- (Feb 13) A Japanese woman in her 80s tested positive after death. Her son- in-law, a taxi driver, also tested positive. He had not travelled to the affected parts of China and denied having carried any foreign customers in the two weeks before testing positive. https://www3.nhk.or.jp/nhkworld/en/news/20200214_15/
- (Feb 16) An 82-year old man in Seoul, Korea, had no record of overseas travel or contact with other positive testing people. https://en.yna.co.kr/view/AEN20200216001355320?section=national/national
- (Feb 16) An 83-year old American woman was screened as disease free after leaving a cruise ship but tested positive twice after arrival in Malaysia. Ironically, her husband had pneumonia, but tested negative. Nobody on the ship was sick, nor had travelled to mainland China recently. https://www.nytimes.com/2020/02/16/world/asia/coronavirus-cruise-americans.html
- (Feb 17) Three men in Aichi, Chiba and Hokkaido prefectures in Japan have no infection routes identified. https://www3.nhk.or.jp/nhkworld/en/news/backstories/878/
- (Feb 18) A 61-year-old woman described as a “superspreader” was the first person diagnosed in her highly populated region of South Korea, with no
known contacts or travel to explain her case. She was blamed for spreading
the infection to 37 other people, but this may just be an artefact of the size of
the church. She had 1,160 “contacts” (presumably mainly members of her
congregation), and so the fraction of cases among her contacts is 3.3%, lower
than the rate of positive tests seen overall in South Korea.
- (Feb 20) JAMA article on original cases in Lombardy reports that none of the 37 cases found within 24 hours had any links to each other or to previous coronavirus cases (e.g. from people arriving to Italy from China) [34].
- (Feb 22) Two cases in Chiba prefecture, Japan, had no relationship with each other, or any contact with other cases or a relevant travel history.
https://www.straitstimes.com/asia/east-asia/japans-new-coronavirus-cases-rise-again-as-doubts- about-prevention-grow
- (Feb 22) Director-General of WHO says that “cases with no clear epidemiological link, such as travel history to China or contact with a
confirmed case” are a concern.
https://www.npr.org/sections/goatsandsoda/2020/02/22/808440540/coronavirus-cases-triple-in- south-korea-who-keeps-eye-on-africa-iran
- (Feb 27) After a hospital in Vienna, Austria, decided to test everyone with compatible symptoms, a 72-year old man tested positive. He had no known
route of infection, had already been in the hospital 10 days, and none of his
contacts were ill or infected. https://www.vindobona.org/article/coronavirus-infected- person-has-been-in-hospital-for-several-days
44
- (Feb 27) An 88-year old man in San Marino (Duchy within Italy) tested positive, but an investigation showed he had not travelled abroad, nor to the
‘red’ areas of Italy where other cases have been found.
https://sanmarinortv.sm/news/comunicati-c9/gruppo-coordinamento-emergenze-sanitarie- aggiornamento-del-27-febbraio-2020-a184304
- (Feb 28) An Oregon resident became the first positive case with no known history of travel to affected countries or contact with infected individuals.
https://www.washingtonpost.com/world/2020/02/28/coronavirus-live- updates/?p9w22b2p=b2p22p9w00098
- (Feb 28) A dog in Hong Kong whose owner was positive, also tested positive, but scientists claimed that perhaps the dog was not infected but had just
inhaled or ingested virus particles. They did not explain why this could not
also occur with humans. https://www.cnbc.com/2020/02/28/a-dog-in-hong-kong-tests- positive-for-the-coronavirus-who-confirms.html
- (Mar 1) Newsweek reported an American man tested negative upon return from Wuhan, China, without any symptoms. But later he was “weakly positive” and was returned to quarantine. https://www.newsweek.com/cdc- mistakenly-released-texas-coronavirus-patient-who-later-tested-positive-san-antonio- mayor-says-1489939
- (Mar 2) A medical article reported a woman in Guangdong, China who tested positive at the end of an 8 day period of symptoms, had two negative tests
after symptoms had resolved (days 12 and 14), but then a positive test (day
17), followed by three more negative tests (days 20, 22, 32). She was
asymptomatic this entire time.
https://www.sciencedirect.com/science/article/pii/S1201971220301223
- (Mar 2) El Pais reported that at least five positive cases in Torrejón de Ardoz, near Madrid, had not travelled to any country considered a risk, not had contact with any other patient. https://english.elpais.com/society/2020-03-02/health- experts-concerned-over-unexplained-coronavirus-cases-in-spain.html
- (Mar 6) British Columbia, Canada reports a positive case with no recent travel history and no known contact with another patient.
https://www.scmp.com/news/world/united-states-canada/article/3073841/coronavirus-british- columbia-announces-canadas
- (Mar 12) A woman returned from Italy to Cuba, where her husband was, and developed minor respiratory symptoms after her return [27]. Her symptoms resolved, but a few days later the husband developed symptoms, and both went to a hospital, where they were put in isolation. When they were tested, the husband, who had not been outside the country, was positive, but the wife was negative. The medical institute hypothesized that she had become negative in the 15 days after her first symptoms, but there was no evidence that she had ever been positive.
45
- (Mar 19) CTV reports on a man with leukemia, who went to a hospital with night sweats and a cough, was given antibiotics and sent home, worsened,
was intubated, and then sadly died. A test result received after his death was
positive. He had not recently travelled or had contact with another
coronavirus patient. https://www.ctvnews.ca/health/coronavirus/stay-home-urges-widow-of- 51-year-old-ontario-man-who-died-of-covid-19-1.4860802
- (Mar 21) Iceland reported that 33.2% of 473 cases had not been conclusively traced to a source of transmission.
https://www.government.is/news/article/2020/03/15/Large-scale-testing-of-general-population-in- Iceland-underway/
- (Mar 25) The urban region of Kitchener-Waterloo in Canada reported that, “For almost all of our recent presumptive cases, there is no link to a previously identified case”. https://www.kitchenertoday.com/local-news/risk-of- contracting-covid-19-present-across-the-region-2198655
- (Mar 26) A New Zealand man suffered bullying after being the first person in his small community diagnosed positive. He felt sick after playing cricket, but all his close contacts, including his cricket mates, have tested negative. He had not been with any international travelers, nor travelled himself. The only possible connection is that 3 weeks earlier he had been at a concert in Aukland where one other person tested positive, but not evidence that the two were ever close, and no explanation of how his disease would have taken 3 weeks to manifest.
https://www.stuff.co.nz/national/health/coronavirus/120584410/coronavirus-bullying-in-the- wairarapa-causes-man-with-the-coronavirus-to-breakdown
- (Mar 30) The family of a 70 year old woman, the first to die in New Zealand, “has no idea how she became infected”.
https://www.stuff.co.nz/national/health/coronavirus/120663168/coronavirus-family-of-the-new- zealands-first-death-have-no-idea-how-she-contracted-covid19
- (Apr 5) A tiger in the Bronx Zoo tested positive, one of 7 animals that developed a dry cough, but the only one to test positive. There was no explanation about how a human got close enough to transmit the virus, whether that person is still alive, and whether they also tested positive for coronavirus. https://nypost.com/2020/04/05/a-bronx-zoo-tiger-now-has-coronavirus/
- (Apr 10) A Yanomami teen in a remote area near the Venezuela-Brazil border region tested positive after reporting shortness of breath and fever. There is
a theory that he was infected by an illegal miner passing through, but no
evidence of any contact. https://www.foxnews.com/world/teen-in-remote-amazonian-tribe- tests-positive-for-coronavirus
- (Apr 10) South Korea reported that 91 patients who had been cleared through negative tests had tested positive again. Official didn’t know if the
virus had been reactivated, the patients had relapsed, the test was measuring
non-infectious debris from the virus, or there were false test results.
- (Apr 10) A 42-year old man with an inherited form of muscular dystrophy died, and the autopsy revealed bronco-pneumonia. While a nasal swab was
46
RNA-positive for COVID-19, lung swabs were negative when tested.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7184436/
- (Apr 15) A 68-year-old Chinese man was admitted to hospital due to fever, muscle pain, and fatigue, and had two consecutive positive coronavirus tests.
He was released after his symptoms resolved and he had two consecutive
negative tests. During a quarantine period he tested positive twice again, and
was re-hospitalized, and given antiviral drugs, despite having no symptoms.
He then had four negative tests and was discharged. But then he tested
positive twice more, still without symptoms, and was hospitalized a third
time, and given antiviral drugs a second time (despite no symptoms). Finally,
he was released into quarantine for a third time. No indication that false
positive results were occurring was mentioned.
- (Apr 18) An article in the International Journal of Infectious Diseases found much higher rates of positive results in nasal swabs than in throat swabs in
353 people who had both samples taken at the same time. Overall 19% of
nasal swabs and 7.6% of throat swabs were positive. This was particularly
pronounced among hospital inpatients (33% versus 9%). The researchers
did not consider that perhaps these people were picking up RNA from the
atmosphere of the hospital. They also concluded that when the results were
contradictory, it was the negative test that was wrong. No reason was given.
- (Apr 29) The number of positive tests in cleared patients in South Korea had risen to 277, and the explanation had changed to the RT-PCR test detecting viral debris: bits and pieces of left-over RNA. However, there was no explanation of why loose RNA would remain the body for so long, nor why the patients would first test negative when they would have had even more of the ‘viral debris’ in their body. https://en.yna.co.kr/view/AEN20200429007051320
- (Apr 19) Taiwan found 21 COVID-19 positive sailors on three naval vessels that had sailed to Palau and back. The infection is believed to have come from
Palau, despite the island nation having reported no cases.
- (May 3) The President of Tanzania sent samples from a goat and a pawpaw fruit to the national lab and they tested positive. On the other hand, a sample from a sheep was negative. https://www.reuters.com/article/us-health-coronavirus- tanzania/president-queries-tanzania-coronavirus-kits-after-goat-test-idUSKBN22F0KF
- (May 5) A Georgia, USA, man tested positive at 8am and then, about 4 hours later, tested negative (he had also tested negative 10 days before).
https://www.fox5atlanta.com/news/cobb-county-man-tests-positive-and-negative-for-covid-19-just- hours-apart
- (May 5) A December 27th 2019 blood sample from a man in France tested RT- PCR positive for COVID-19. This lead doctors to postulate that the virus was circulating earlier in France. They did not consider the possibility that it was a false positive, especially because the man had not recently travelled, nor is known to have come into contact with someone from Wuhan which, according to COVID-19 dogma, was the only location of the virus at that time.
47
https://www.livescience.com/coronavirus-france-patient-zero-december.html (Jan 31) A
women returning to Canada from China tested negative while “mildly ill”
after arriving in Canada, but later tested positive.
https://www.theglobeandmail.com/canada/article-fourth-case-of-novel-coronavirus- confirmed-in-canada/
- (May 13) Janice Brown, a woman with a medical history of cancer, strokes, heart attacks, renal failure and congestive heart failure, spent 2 months in a
hospital as a COVID-19 patient. After she had been symptom free for 3 days,
she was discharged on April 3rd, but on April 21st, she had problems during
dialysis and was re-hospitalized, and tested positive again. Finally, she tested
negative again and was released a second time.
https://www.latimes.com/california/story/2020-05-13/coronavirus-test-second-infection-hospital
- (May 6) New York Presbyterian laboratories found 49 people whose results went from RNA positive to negative and back to positive (sometimes more than once) out of 3,432 people who were repeat tested (but most who were repeat tested were only tested twice, so this phenomenon would not be visible). They also had 1.6% of tests come back ‘indeterminate’ (neither positive nor negative). https://www.medrxiv.org/content/10.1101/2020.05.06.20093575v1
- (May 8) 5 sailors aboard US aircraft carrier “Roosevelt” tested positive for coronavirus a second time. John Swartzberg, a UC Berkeley infectious disease expert was quoted as saying, “This is not behaving like any infectious disease I have heard of, if these tests are accurate. None of this makes any sense.”
https://www.sfchronicle.com/bayarea/article/Five-sailors-aboard-Roosevelt-carrier-retest- 15273804.php
- (May 18) 33,000 Floridians may have received positive RNA test results when they were negative, or negative results when they were positive, or no
results at all, due to incompetence by a contractor.
https://www.wfla.com/community/health/coronavirus/33000-floridians-who-took-covid-19-test- may-have-incorrect-results-adventhealth-says
48
Appendix B Revision History
Revision Major changes
| 6.2 | False positives: Chinese paper documenting 80% false positive rate. Transmission 5: Illinois couple, first community transmission in US. Treatment: Completely reorganized and updated. Treatment experience: Information from Italy deaths and Wuhan patient. |
| 6.3 | Revision History added. Information from Diamond Princess analysis. Correct link to Chinese false positive paper. |
| 6.4 | Numbered sections. Replaced news report of Italian deaths by official ISS report, updated with many more patients, in the Treatment section. Split off first part of “Treatment Experience” into “Patient Status”. |
6.5 Moved ‘magical transmission’ cases to Appendix A and added another case. Moved ‘Preserve the test” cases to Appendix B.
| 6.6 | Reorder appendixes in same order as text. Moved ‘Confusing Test Results’ to Appendix A. Fix all hyperlinks from URLs in reference list. |
| 6.7 | Comments from Dr. David Rasnick. Put Executive Summary first. Expand comments on false positive study now English translation is available. Added report on Italian cluster of 37 disconnected cases to ‘magic transmission’. |
| 7 | Add link to English version of ISS report. Add more drugs, and information on usage in Italy, to Treatment section (Tocilizumab etc). Add failure of Chinese Kaletra (Lopinavir+Ritonavir) drug trial. Under Treatment, new section on invasive ventilation, including VALI and VAP. Add links in appendixes, to original news articles, where no reference is provided. Add footnotes for RNA and the retraction of the abstract of the Chinese false positive paper. |
7.1 Corrections to invasive ventilation section.
| 7.2 | Moved Revision History to an appendix. Clarify that the paper is not advocating people going to an ER with minor symptoms. Add Austria testing statistics. Add references to the invasive ventilation section to show recommendations to rapidly intubate and avoid non-invasive ventilation. |
| 8 | New chapter on Mortality. Expanded information on RT-PCR testing for coronavirus, including review of 33 FDA approved test. More information on people who tested positive again after being cleared as negative. UK and New York data on characteristics of coronavirus positive people who died. Expanded information on treatments. |
| 8.1 | Remove section on panic disorders and hypoxia as this does not appear to be widely supported. Add information on corticosteroids. Hydroxychloroquine can be dangerous to people with modified G6PD gene, mostly Africans. Gilead changed remdesivir trial to remove death as a primary end point. Note that the Chinese woman in the German cluster did actually have mild symptoms during the meeting in Germany. |
49
| 8.2 | NEJM paper with risks for mortality. Paper comparing rate of positives among nose versus throat swabs. 66% of new cases in New York as of early May were people who had stayed home (retired or unemployed). |
| 8.3 | Tanzania false positives on fruit and goats. Georgia positive and negative test on same day. NY State hydroxychloroquine/azithromycin study. Information on Vitamin D insufficiency. California woman Janice Brown tests positive again after release from hospital. Merge Appendixes A, B and C, as there is so much overlap with ‘impossible’ test results. Chinese study on hydroxychloroquine. |
| 8.4 | Update to Italian ISS study on COVID-19 mortality. Lancet study on chloroquine and hydroxychloroquine death and heart arrythmias. Chinese patient with 455 contacts, all RNA-negative. Spanish and Swiss palliative care documents. Correct wrong figure in Vitamin D study, and include reference number in text. Fix and clarify math and wording in false positive section, including population of Wuhan. WSJ article on increases in prescriptions for anti-anxiety drugs and sleeping pills. |
| 8.5 | Italian data on social connectedness. Canadian Forces letter on severe deficiencies in 5 care homes in Ontario, Canada. Removal of two studies with probably fraudulent data from Surgisphere. JAMA survey on psychological distress. BMJ paper on testing with reference to gold standard. JAMA study on advanced non-invasive intubation. |
50
Original Article: https://prepareforchange.net/2021/02/15/flaws-in-c-pandemic-theory/?utm_source=rss&utm_medium=rss&utm_campaign=flaws-in-c-pandemic-theory
Related posts:
Views: 0
 RSS Feed
RSS Feed

















 February 16th, 2021
February 16th, 2021  Awake Goy
Awake Goy  Posted in
Posted in  Tags:
Tags: 
















