Global Excess Mortality Rates — Where’s the Investigation?
Are scientists and the media deliberately overlooking COVID-19 vaccines as a possible factor in global excess mortality rates?
By
Rob Verkerk Ph.D.
Miss a day, miss a lot. Subscribe to The Defender’s Top News of the Day. It’s free.
We have previously pointed to official data in 2021 that shows a temporal association between the apparent rises in “excess mortality” among different age groups and the time each was exposed to COVID-19 “genetic vaccines” (here and here).
These data were in plain sight in the public domain, being based on official data from the nearly 30 mainly European countries carried on the euroMOMO portal.
Now, a year on, it’s nigh on impossible to hide the fact that in many industrialized countries that went full swing into intense control measures, from lockdowns, masks, genetic surveillance and “genetic vaccines,” people are dying at unexpectedly high rates.
The jabs or boosters may be a factor — but so may a bunch of other things, such as not gaining timely and proper medical attention, psychosocial stress and deprivation, along with a gamut of other potential co-factors.
The current apparent excesses in deaths over those that would have been expected is especially unusual given they have occurred during the northern hemisphere summer when deaths are normally at their lowest — and it is difficult to apportion blame to an invisible virus that on all accounts has lost virulence in its current guise.
According to The Guardian, even the U.K. Health Security Department argues summer heatwaves only explained around 7% of the excess mortality in July in England and Wales.
We have to ask ourselves what’s really going on.
Are the statistics tricking us, or is there something ominous going on that’s not being reported?
If the latter, how much effort is going into trying to unearth the causes of these deaths — and how many are, or could be, preventable?
From unadjusted mortality to excess mortality — the imperfect but perhaps best metric we have?
At Alliance for Health International, we’ve been tracking mortalities in different countries, especially “excess mortalities,” for the last two and half years (e.g. here and here).
For anyone who might need reminding, “excess deaths” is a term used in epidemiology and public health that refers to the number of deaths from all causes, beyond what we would have expected to see under “normal” (in this case the most recent pre-pandemic) conditions.
Straight all-cause mortality data is not a great metric on its own as it fails to take account of the population size (which is in turn affected by birth rate, death rate, immigration and emigration) or the age structure in a given country.
Countries with top-heavy age structures, like many industrialized ones, will have much higher expected mortality rates than those populated mainly by younger age groups, such as so-called “less developed countries.”
If a crisis, like COVID-19, causes women to give birth to fewer children (owing to the conditions of the crisis, impacts on fertility or any other cause), unadjusted mortality data per 100,000 population will appear to rise, but this apparent rise is a statistical artifact.
Factors like age, population size, ethnicity and socioeconomic status can of course be standardized or adjusted for, but you still don’t get a broad picture of what’s going on at a population, national or international scale, because your adjustments have forced you into looking at specific segments of the population.
Excess mortality is widely recognized as one of the most important markers of crisis-related changes in mortality.
This is because it compares mortalities for a given population size and structure in the crisis against those that would be expected in the same country derived usually from the average of the most recent few (often 5) non-crisis years.
The fact that this metric doesn’t get affected by things like how or why COVID-19 deaths are recorded on death certificates, and it is specific to the particular demographics and age structure of the country in question, has led to it becoming widely regarded as a robust marker — even a gold standard — for assessing the impact of the COVID-19 crisis.
If only it were that simple.
Different countries report their own data at different frequencies — or not at all.
Different groups of researchers also use different statistical methods and parameters to derive excess mortality, these often not being reported in sufficient detail to really understand how they’ve come up with their numbers.
Thus failing in the important scientific reporting principle that says that other scientists should be able to reproduce the same results with the same data.
Something that particularly bugs me is that those reporting excess mortality fail to explain exactly where and how they sourced their non-crisis comparator data.
As German scientists Christof Kuhbandner and Matthias Reitzner rightly indicate in their recent preprint study of excess deaths in Germany between 2020 and 2022 (discussed below):
“While the number of observed all-cause deaths is a fixed and clearly defined number, the estimation of the usually expected deaths is relatively complex and entails several choices of mathematical models and parameters and which can lead to large differences in the estimated values.”
Totality of evidence
So, like all statistics, excess mortality data may still mislead.
But before we throw this metric in the nearest recycling bin, let’s pay homage to another scientific principle — that is, especially when uncertainty abounds (yip, that’s us on this issue, folks), reserving any conclusions until the totality of available evidence has been assessed.
This, in essence, means not cherry-picking your data, and instead, looking at all plausible data and analysis, interpreting it and only then drawing conclusions from it.
This is why I implied earlier that it’s now becoming very difficult to hide the fact that something ominous is going on with all-cause or excess mortality.
We know now from multiple sources of official data from different countries that COVID-19-related deaths aren’t much of an issue at present, such as the lack of virulence of the circulating Omicron strains (something that might change given the selection pressure that is likely to ensue as more people opt for “genetic vaccination” this autumn).
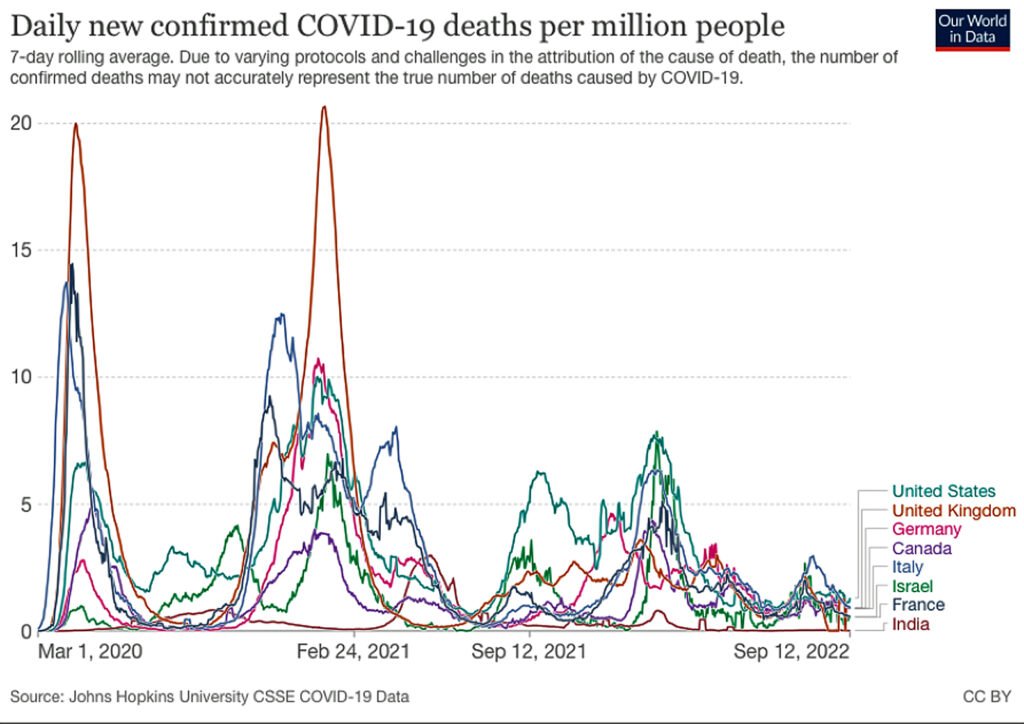
Bear in mind, even these “COVID-19 deaths” (as tracked globally through Our World in Data, see Fig. 1) have often substantially overestimated deaths because COVID-19 was in the majority of occasions not found to be the primary cause of death.
Rather, it was only associated with deaths, having been determined by way of a flawed PCR test within, say, one month of death.
Yes, someone killed in a motorcycle accident who died 27 days after having received a false positive COVID-19 antigen test would be down in the official record as a “COVID-19 death.”
Figure 1. Confirmed deaths per million population from selected countries. Credit: Our World in Data
Multiple sources, all pointing to an unexpected rise in deaths in 2022
The following are five important sources that include country-specific, region-specific and global data that most reputable scientists (an ever more tricky characterization), I believe, would regard as being of high quality, and approaching the “totality of evidence” threshold, that we think paint a fairly complete picture of the excess death paradox we currently face.
1. Excess mortality data for England, from the Office for Health Improvement and Disparities (U.K.)
The first thing to note is the relative increase in excess mortality over the three successive summers (Fig. 2).
Figure 2. Excess mortality in England between February 2020 and August 2022. Red notations added by the author. Source: Office for Health Improvement and Disparities. Methodology is given in a link in the second paragraph of the Introduction in the above document.
More than this, when you explore the data from this Office for Health Improvement and Disparities source, you find that some of the biggest excesses compared with expected deaths have occurred in the two youngest age groups, ages 0 to 24 years and 25 to 49.
Not only that, there are few differences in death according to the level of deprivation, which might have been caused by inadequate or poor quality diets or lifestyle effects.
Ethnicities also had an influence with white and mixed ethnicities being most impacted, while black and Asian ethnicities, were least affected.
This pattern, whether or not it is coincidental, follows the pattern of COVID-19 “vaccine” uptake — Johnson’s government pushing hard but ineffectually to get black and Asian ethnicities to be less “hesitant.”
There were also some differences in region, and it’s of interest that low COVID-19 “vaccine” uptake and highly polluted London had the lowest excess mortality of any of the regions.
2. Excess mortality from Germany, 2020-2022
In their ResearchGate preprint analyzing excess mortality in Germany between 2020 and 2022, Christof Kuhbandner (University of Regensburg) and Matthias Reitzner (University of Osnabrück) have applied actuarial science to get to the bottom of the excess mortality figures in Germany.
Long and short of it — with different, interesting and transparent methodology — here are some of the top line findings:
- In 2020 there was no apparent significant excess mortality.
- Excess mortality started rising as of April 2021 for reasons other than COVID-19 caused or associated mortality.
- Nearly all of these excess deaths were in the age groups between 15 and 79 — hence not including the oldest most frail members of society that have historically been shown to be the most likely to succumb to respiratory infections.
3. EuroMOMO — regional excess mortality data mainly from Europe
Readers and supporters of Alliance for Health International have been led by us so often to the euroMOMO website.
That’s the deal — we have to keep looking as every time we look, we get to see a snapshot in time. We only start to get a more complete picture of what’s going on when we see all the snapshots together in our “COVID Crisis Album.”
The excess mortality in the youngest age group across all 28 euroMOMO countries/regions continues for 2022 and is deeply disturbing as it includes the youngest and most vulnerable in society between the ages of 0 and 14 years.
But there is a noticeable trend for excesses that have occurred at a time when Omicron has caused little in the way of mortality, in a number of countries.
Let’s look at these data in two ways via the graphs and maps section of the euroMOMO website.
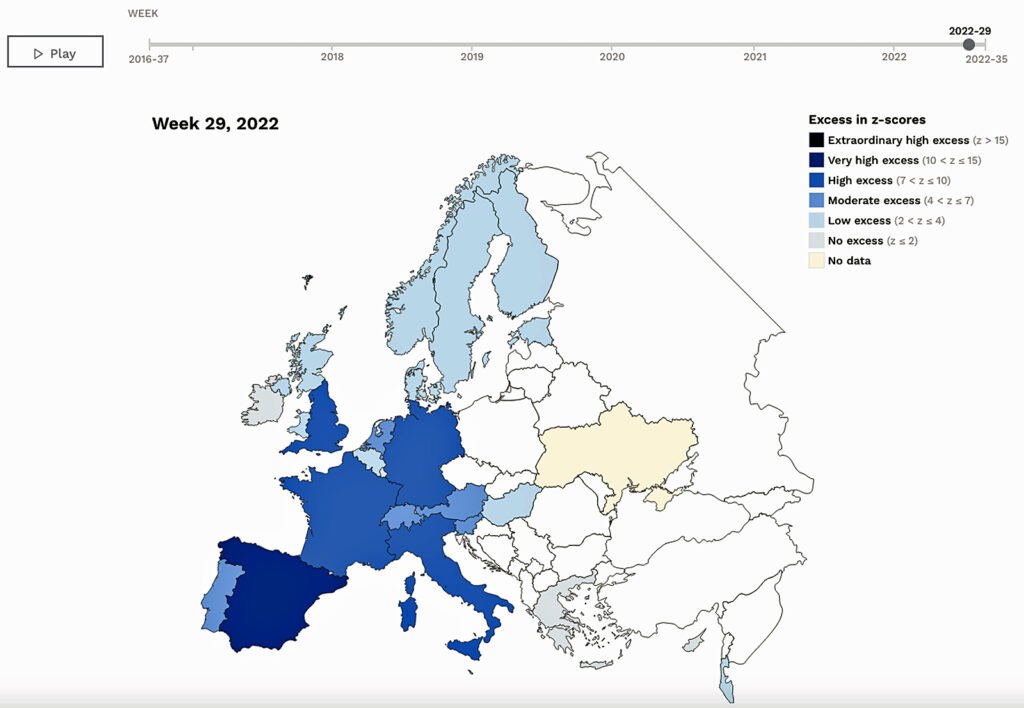
Firstly, scroll down to the “Map of z-scores by country” (z-scores being the specific excess mortality used by euroMOMO based on a published method), and then move the time slider to see the most recent few weeks over the summer of 2022.
“Houston…”, or should I say, “… Ursula von der Leyen, we have a problem, even if you don’t want to talk about it.”
Following (Fig. 3) is a screen grab from a single time point of week 29 (third week of July) where you can see high excess mortalities in England, France, Germany and Italy, with very high excesses in Spain.
As noted earlier, this cannot just be a heatwave effect.
Figure 3. Excess mortalities (as z-scores) in Europe during week 29 (July 18-24) 2022. Credit: EuroMOMO.
Secondly, check out the age data under the Excess mortality heading (Fig. 4). You’ll see marked excesses in both the 0-14 and 15-44 age groups in 2022, ones that were comparatively affected by the initial pandemic waves in 2020.
This is particularly disturbing as the effect is not even diluted by those countries that didn’t have serious COVID-19 burdens (e.g. much of Scandinavia).
Figure 4. Excess deaths for all age groups, and the youngest two age groups in the complete euroMOMO cohorts (including all 28 partner regions/countries). Credit: EuroMOMO.
You can even look at it in a third way, via the country graphs at the base of the page, which will show you the upticks we saw via the “Map of z-scores by country.”
4. Our world in data — national and global excess mortality data
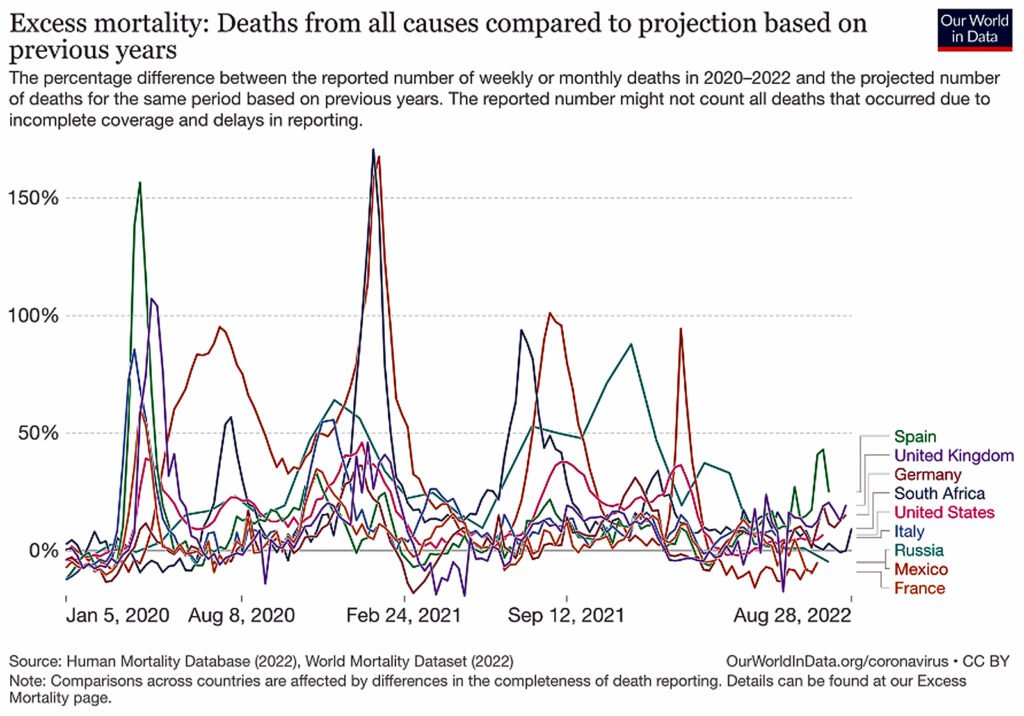
I’ve long been bemused that excess mortality — this very robust statistic, sits at the end of all the various statistics that Our World in Data, supported by Johns Hopkins and the Gates Foundation, have assembled in the “data explorer” segment for under the “coronavirus” heading for our viewing pleasure.
I’m also interested that the default countries of late have been three countries the official data from which don’t show significant excess mortality at present, namely Russia, Mexico and South Africa.
Lo and behold, when we add a few more countries in — some that we’ve talked about above, we see the same trend in rising excess mortalities (Fig. 5).
Figure 5. Excess mortalities from selected countries based on official data analyzed by Our World in Data. Credit: Our World in Data
5. The Economist machine learning algorithm for national and global excess mortality data
The final data source I’m going to touch on is the excess mortality data being churned out of the state-of-the-art, machine learning algorithm developed by The Economist.
The unique methodology used factors in over 100 variables, it teases out those that don’t have much influence, it estimates data from similar countries, regions and demographics where data are missing and appears to try pretty hard to give us as complete a picture that available data and science-based estimates allow.
The first thing to notice about The Economist’s tracker is that excess deaths during the pandemic period are way higher than the official deaths.
The official death toll is currently cited as 6.5 million — the Economist’s algorithms roughly triple this, suggesting a more likely, actual death toll of between 16 and 27.2 million.
It seems likely that if these estimates are more realistic, many of them won’t be directly attributable to a virus.
Estimated cumulative deaths globally deliver something of a pessimistic picture, with many parts of the world from the U.S., most of South America, Russia, Eastern Europe, Italy, Greece, India and South Africa all experiencing considerably more deaths than would have been expected in the absence of a pandemic and measures deployed ostensibly to protect public health (Fig. 6).
Figure 6. Global cumulative excess mortality assessed from March 2020 through to the present. Credit: The Economist.
This cumulative perspective, of course, doesn’t show us what’s going on now.
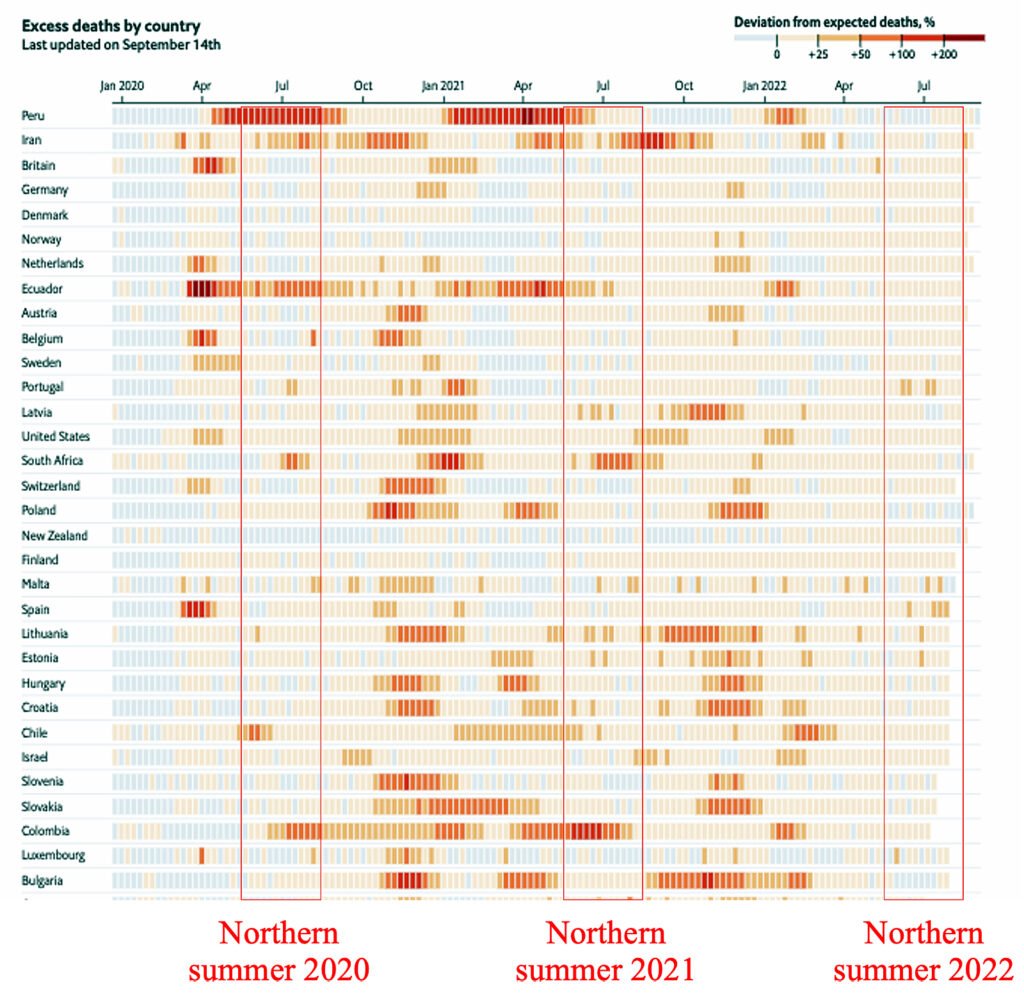
Here (see rectangle highlighting “Northern summer 2022” in Fig. 7) we can see the previously discussed pattern of excess mortalities, within the 0-25% excess range, for many (not all) countries, regardless of them being northern or southern hemisphere, especially those with more complete data sets (Fig. 7).
Figure 7. Excess mortality tracker showing selected countries and nearly fully consistent pattern of excess deaths (highlighted by red rectangles; our addition) shown as light or dark amber. Credit: The Economist COVID-19 excess mortality tracker.
When comparing excess mortalities of the northern summer of 2022 with those of 2021 and 2020, we see the more expected patterns that have been widely associated with discrete, somewhat seasonal waves of SARS-CoV-2 infection hitting countries at different times.
The southern hemisphere appeared to be affected to a greater extent during its own winter, which corresponded to the northern hemisphere summer.
This trend appears to have dissipated by the summer of 2022, but rather than returning to baseline, pre-pandemic mortalities in line with the recent loss of SARS-CoV-2 virulence, significant excess mortality is still noted, irrespective of hemisphere.
What’s killing people?
“They” — including the mainstream science and medical establishment, governments and much of the media — are largely mute on trying to unpick what’s going on.
When they do recognize the paradox of excess mortalities now that the pandemic is viewed by most as largely over or in a temporary lull prior to another assault this northern hemisphere Autumn, the one consistent thing you find is the lack of any mention of the possible role of those infernal “genetic vaccines.”
This shouldn’t be a surprise given the extraordinary suppression of information on the scientific discourse around these gene-altering products, as reported by Ety Elisha, Josh Guetzkow and colleagues in the peer-reviewed journal HEC Forum that has been informed by the forcibly released Pfizer data that reveals just how much the regulators knew about lack of effectiveness and significant harms when they issued emergency authorization in 2020.
Among those acknowledging excess mortalities, Professor Devi Sridhar, chair of global public health at the University of Edinburgh, is typical in her inability to consider the “vaccines” as a possible determinant in the current rise in deaths.
In a recent article in the Gates-funded Guardian newspaper, COVID-19 still held the limelight as a key determinant, despite little in the way of supporting evidence.
In professor Sridhar’s own words:
“It’s likely to be a mix of factors: COVID is making us sicker and more vulnerable to other diseases (research suggests it may contribute to delayed heart attacks, strokes, and dementia); an aging population; an extremely hot summer; and an overloaded health service meaning that people are dying from lack of timely medical care.”
What’s the real mix of contributory factors?
Honestly? We don’t know! But we could add a few additional points to Prof Sridhar’s list that might be worth looking into, should any researchers be interested (but who will fund them?):
- Suicides.
- Loneliness.
- Depression and anxiety.
- Lack of purpose or meaning in life.
- Inappropriate diets.
- Inappropriate lifestyle.
- Breakdown in social relationships.
- Lack of timely access to effective healthcare services.
- Lack of early diagnosis of serious, life-threatening conditions or diseases.
- Short, medium and longer-term harms of “genetic vaccines.”
- Increased autoimmune diseases triggered by “genetic vaccines.”
- Increased infectious disease prevalence from compromised immunity from social isolation and “genetic vaccines.”
- Enhancement of chronic diseases by dysregulated immune system and persistent systemic inflammation, triggered by repeated exposure to COVID-19 “genetic vaccines.”
- Sub-optimal treatment of COVID-19 disease (e.g. remdesivir).
- Failure to implement effective early treatment (e.g. as per FLCCC [Front Line COVID-19 Critical Care Alliance] protocols).
- Inappropriate use of mechanical ventilators.
- Unwarranted placement of DNR (“do not resuscitate”) notices on care home residents.
- Unjustified use of powerful sedatives (e.g. midazolam) known to contribute to deaths in nursing homes.
Even this is a partial list, supplementary to that of Prof Sridhar.
However, in light of what we know now about COVID-19 “genetic vaccine” harms, their omission as potential contributors to the clearly evident excess mortalities in many countries is a grave — and likely deliberate — scientific oversight.
An oversight that is likely killing and injuring people, unnecessarily.
Society normally has ways of dealing with deliberate oversights of this nature, through the courts and penal system.
Maybe that’s still to come?
If there’s one feeling I have about any retribution, it is that in the years to come, this omission and violation of human rights and human life will be seen for what it is by the majority, not just a growing minority.
Originally published by Alliance for Natural Health International.
https://childrenshealthdefense.org/defender/global-excess-mortality-rates-deaths/?utm_source=salsa&eType=EmailBlastContent&eId=6f75c9ff-f264-4374-99bc-3da7072bce23
Thanks to: https://childrenshealthdefense.org
Related posts:
Views: 1
 RSS Feed
RSS Feed

















 September 23rd, 2022
September 23rd, 2022  Awake Goy
Awake Goy 



 Posted in
Posted in  Tags:
Tags: 
















